Articles
- Page Path
- HOME > STRESS > Volume 29(2); 2021 > Article
-
Original Article
병원 근무 간호사를 위한 의사소통 역량향상 프로그램에 대한 체계적 고찰 -
전예슬
 , 최희승
, 최희승
- A Systematic Review of Communication Programs for Nurses Working in Hospitals
-
Yeseul Jeon
 , Heeseung Choi
, Heeseung Choi
-
stress 2021;29(2):69-79.
DOI: https://doi.org/10.17547/kjsr.2021.29.2.69
Published online: June 30, 2021
1 서울대학교 간호대학
2 서울대학교 간호과학연구소
1College of Nursing, Seoul National University, Seoul, Korea
2The Research Institute of Nursing Science, Seoul National University, Seoul, Korea
Copyright © 2021 by stress. All rights reserved.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 3,237 Views
- 392 Download
- 3 Crossref
Key messages
- 본 연구는 병원 근무 간호사를 위한 의사소통 프로그램의 특성과 효과를 탐색하기 위해 시행된 체계적 문헌고찰이다. 국내외의 5개 데이터 베이스(PUBMED, EMBASE, CINAHL, PsycINFO, RISS)를 활용하여 최근 10년간 발표된 문헌을 추출한 후 분석하였다. 주요 검색어는 간호사, 의사소통 등이었으며 총 13편이 포함되었다. 프로그램은 강의, 시뮬레이션, 디브리핑 등의 다양한 활동을 했으며, 대부분의 연구에서 의사소통역량이 향상되었다. 향후 다양한 부서의 상황을 반영한 시뮬레이션을 개발하여 그 효과를 살펴봐야 한다. 또한 도구를 결정할 때 연구목적에 따라 참여자의 자가보고에 따른 주관적 평가도구와 함께 관찰자를 통해 확인된 참여자의 행위변화와 같은 객관적 평가도구의 사용을 고려해야 한다.
Abstract
-
Background
- Despite the implementation of several communication programs for nurses working in hospitals, no evidence-based systematic review has yet been conducted on their efficacy.
-
Methods
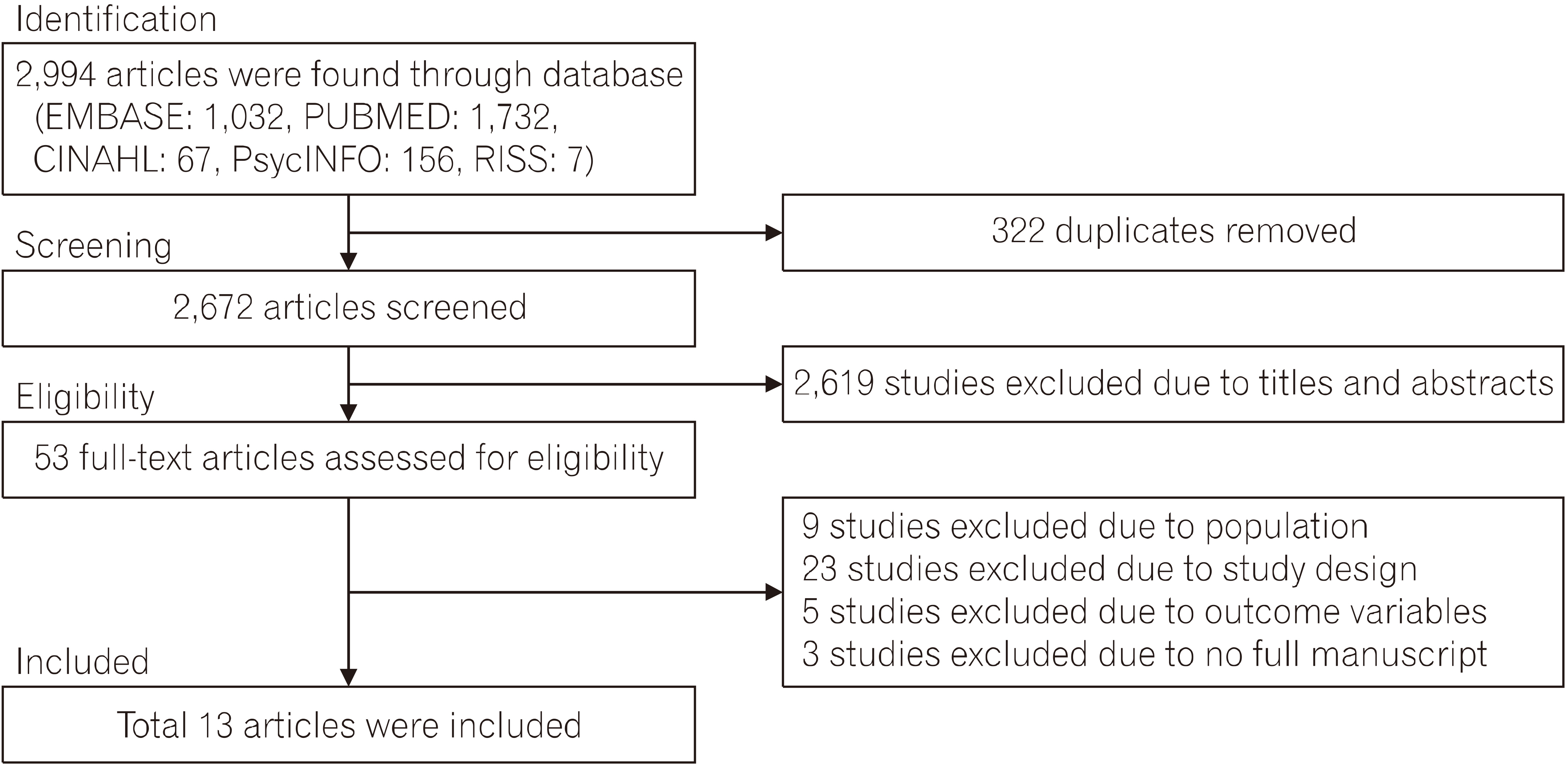
- In this systematic review of communication programs for nurses, we searched for literature published between 2011 and 2020 in four foreign databases and one domestic database (PubMed, Embase, CINAHL, PsycINFO, and RISS). The papers identified were evaluated on their quality using Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2). The main search terms included “nurse”, “communication”, “program”, and “intervention.” Thirteen articles were included in the final analysis.
-
Results
- The communication programs utilized various teaching methods – such as simulation, reflection, and debriefing – with a majority of these programs significantly improving participants’ communication skills and performance. However, the overall quality of the studies was low concerning the randomization process and measurement; relatively few studies made use of online education methods. All variables assessed using self-reported measures were significant, but not all showed significant results when using objective measures as assessed by the evaluators.
-
Conclusions
- The study’s findings suggest a need for programs dealing with nurses’ communication with health care providers in diverse clinical settings and online-based simulation programs. Moreover, high-quality literature applying the randomization process and measurement is required. Additionally, it is necessary to use both subjective and objective measures to evaluate the overall communication capacities of nurses and reflect the contextual characteristics of various clinical settings.
- 의료현장에서 간호사의 주요업무는 대상자와의 상호작용을 통해 대상자의 기대와 요구에 따라 대상자를 관리하고 교육하는 것인데, 이때 가장 필요한 능력이 의사소통 역량이다[1]. 또한, 병원에서 근무하는 간호사는 환자뿐 아니라 보호자, 동료 의료진 및 기타 부서의 다양한 종사자들과 관계를 맺고 업무를 조정해야 하므로 간호사의 의사소통기술은 간호사가 갖추어야 하는 필수역량이다[2].
- 효과적인 의사소통은 간호사의 직무 만족도, 팀 관계 그리고 환자의 회복과 안전에 긍정적인 영향을 주는 반면[3], 의료진간의 의사소통 부족뿐 아니라 의사와의 수직적, 비주장적 의사소통을 경험할수록 간호사의 이직의도가 높은 것으로 나타났다[4,5]. 게다가 타 부서 종사자들과의 업무조정 시 의사소통이 미흡할수록 환자안전과 건강에 위협이 되는데[5], 이는 결국 환자의 전반적인 치료과정과 간호직의 전문성에 악영향을 미치기 때문에 간호사들의 의사소통기술을 증진시키는 것은 중요하다.
- 그러나 간호사들의 의사소통기술은 대부분 학부 때 학습한 의사소통 교과목을 기반으로 하고 있다[2]. 이 시기에 의사소통 관련 이론, 치료적 의사소통, 리더십에 대한 교육을 받았으나 이론 교과목이 가지는 한계점으로 실무에까지 연결되기 쉽지 않으며 복잡한 임상현장을 모두 담기에는 어려움이 있다[6]. 또한, 간호사들을 대상으로 한 의사소통 교육은 단발성 강의 위주의 교육방법이 대부분이라 임상현장에서 의사소통역량을 발휘하기 쉽지 않다[2]. 특히, 신규 간호사들이 임상에서 적응하는데 필요한 효과적 의사소통역량에 대한 요구는 높아지고 있으나 실제적으로 실무에서 적용할 수 있는 지속적인 교육과 훈련이 부족한 실정이다[1,2].
- 이러한 상황에서 간호사들의 의사소통역량에 대한 중요성은 점차 강조되고 있으며, 이를 반영하듯 간호사들을 위한 의사소통역량 증진 프로그램이 양적으로 증가하고 있는 추세이다. 국내에서는 이론강의, 역할극(role-play), 토의, 디브리핑, 팀 활동, 사례 기반, 시뮬레이션의 방법을 병용하여 Situation, Background, Assessment, Recommendation (SBAR) 프로그램, 자기주장 훈련 프로그램, 비폭력 의사소통 교육 등의 연구들을 시행하였다[7-13]. 국외에서 간호사를 대상으로 시행한 의사소통 프로그램을 살펴보면 이론 강의, 역할극, 연극치료 기법의 적용, 온라인 매체 활용, 시뮬레이션, 팜플렛, 반영(reflection), 피드백과 토의, DVD 보기 등의 방법을 적용한 연구들이 있었다[14-24]. 이와 같이 국내외에서 간호사를 대상으로 시행한 의사소통 프로그램은 대부분 통계적으로 유의한 효과가 있었으나 각 부서의 상황과 특수성을 반영하였기에 프로그램을 구성하는 개념과 근거가 일정하지 않았으며, 연구자마다 사용하는 도구와 연구 참여자 그리고 측정기간 등이 다양한 것으로 나타났다. 이에 따라 의사소통 프로그램의 내용, 효과 및 동향을 종합적으로 검토하고 통합하여 추후 간호사 대상의 의사소통 프로그램 개발을 위한 최상의 근거를 마련하고자 한다.
- 간호사 대상의 의사소통 프로그램에 대한 동향을 조사한 선행연구를 살펴보면 국내에서 시행한 체계적 문헌고찰은 없었다. 의사소통 프로그램의 효과를 파악하는 국외연구들을 살펴보면 환자안전을 위한 자기주장 의사소통 프로그램, 환자안전 증진을 위한 SBAR 프로그램, 의사소통기술 향상에 대한 교육 프로그램 등과 같이 다양한 의사소통 중재의 내용과 효과를 비교 및 분석한 것이 아니라 주로 한 종류의 프로그램을 대상으로 그 효과를 분석한 경향이 있었다[25-27]. 또한, 연구결과로 상반된 결과(효과있음/효과없음)를 보고하였고 질 높은 문헌의 부족(low-modest)을 확인하였으며, 각 프로그램마다 구성, 내용, 결과 등이 상이한 것으로 나타나 다양한 의사소통 프로그램의 내용과 효과를 체계적으로 고찰하는 것이 필요하다[25-27].
- 따라서 본 연구에서는 병원에서 근무하는 간호사들의 의사소통역량의 향상을 위해 국내외에서 시행한 프로그램들을 종합적으로 살펴본 후 효과를 확인하고 참여자의 특성, 프로그램의 근거, 프로그램의 구성, 프로그램의 변수 및 효과 등의 구체적인 특성과 연구의 동향을 파악하여 추후 의사소통 역량 증진 프로그램 개발을 위한 토대를 마련하고자 한다.
- 본 연구는 국내외에서 2011년 이후로 병원에서 근무하는 간호사의 의사소통역량을 증진하기 위해 시행된 중재연구를 대상으로 ‘체계적 문헌고찰’을 시행함으로써 프로그램의 특성과 효과를 종합적으로 검토하고자 한다.
- 구체적인 목적은 다음과 같다.
서 론
- 1. 연구 설계
- 본 연구는 병원에서 근무하는 간호사들을 대상으로 시행한 의사소통 프로그램의 특성과 효과를 확인하여 최근 10년간의 연구동향을 파악하기 위한 체계적 문헌고찰 연구이다.
- 2. 문헌 검색
- 본 연구는 National Evidence-based Healthcare Collaborating Agency (NECA)에서 제시한 체계적 문헌고찰 매뉴얼에 따라 수행되었다[28].
- 체계적 문헌고찰의 기술 형식인 PICOTS-SD을 기반으로 하여 문헌을 선정하였다. 연구대상(Participants)으로는 병원현장에서 근무하는 간호사를 포함하였고, 중재(Interventions)로는 의사소통 역량 증진을 위한 중재연구로 강의, 사례 기반, 역할극, 시뮬레이션, 웹 기반, 반영 등의 교육방법을 활용한 연구를 포함하였다. 대조군(Comparisons)이 있는 연구를 포함하였으며, 대조군의 조건으로는 의사소통 프로그램 중재를 실시하지 않고 일반적인 교육이나 강의를 실시하였거나 wait-list 그룹을 대조군으로 설정하였다. 중재결과(Outcomes)로는 프로그램의 효과를 의사소통 관련 변수인 의사소통의 질, 의사소통지식, 의사소통기술, 의사소통 자기효능감(communication self-efficacy), 의사소통유능감(communication competence), 공감, 실제 행동(performance or behavior)의 변화 등을 통해 양적인 수치로 표현하여 통계적 유의성을 검증한 연구를 포함하였다. 추적관찰기간은 중재 전후, 그리고 12개월까지 추적관찰한 연구를 포함하였다. 세팅(Setting)으로는 의료현장에서 간호사를 대상으로 하여 프로그램을 진행한 기관을 포함하였으며 무작위 대조 연구 설계(Study designs)를 적용한 연구를 포함하였다.
- 본 연구는 2011년 1월부터 2020년 11월까지 최근 10년간 출판된 국내외 문헌 중 병원에서 근무하는 간호사를 대상으로 시행한 의사소통 프로그램을 조사하였다. 주요 웹 기반의 데이터베이스를 중심으로 문헌검색을 시행하였고, 총 5개의 데이터베이스가 사용되었다. 국외 데이터베이스는 PUBMED, EMBASE, CINAHL, PsycINFO로 총 4개를 선택했으며, 국내 데이터베이스는 학술연구정보서비스(RISS)로 1개를 선택했다. 문헌검색에 사용된 주요 검색어로는 국외의 경우 ‘nurse’, ‘communication’, ‘program’, ‘intervention’ 등을 조합하였으며 국내의 경우 ‘간호사’, ‘의사소통’, ‘중재’, ‘프로그램’ 등을 조합하여 검색했다. 주요 검색어에 따라 작성된 검색식은 다음과 같다.
- (“nurses” [MeSH Terms] OR “nurse*” [Title/Abstract]) AND (“communication” [MeSH Terms] OR “communicat*” [Title/Abstract] OR “convers*” [Title/ Abstract] OR “assertive” [Title/Abstract] OR “speak up” [Title/Abstract] OR “SBAR” [Title/Abstract] OR “scenario*” [Title/Abstract] OR “role playing” [MeSH Terms] OR “role play*” [Title/Abstract]) AND (“computer simulation” [MeSH Terms] OR “simulation training” [MeSH Terms] OR “simulation*” [Title/Abstract] OR “train*” [Title/Abstract] OR “internet based intervention” [MeSH Terms] OR “intervention*” [Title/ Abstract] OR “education, nursing” [MeSH Terms] OR “educat*” [Title/Abstract] OR “program evaluation” [MeSH Terms] OR “evaluat*” [Title/Abstract] OR “program*” [Title/Abstract]) AND “control” [Text Word]
- 논문 검색은 2020년 10월부터 2020년 11월까지 약 30일 동안 시행하였다.
- 본 논문은 2011년 1월부터 2020년 11월까지 국내외 학술지에 출판된 문헌을 대상으로 분석을 하였으며, 대상 논문의 선정기준은 다음과 같다. 영어 혹은 한국어로 작성되었으며, 병원 환경에서 근무하는 간호사를 대상으로 의사소통 프로그램을 적용한 중재 연구이다. 학위논문이거나 학교나 지역사회 환경에서 근무하는 간호사를 대상으로 의사소통 프로그램을 적용한 중재 연구 혹은 의사소통 프로그램의 목적이 의사소통역량 증진이 아닌 환자의 건강 관련 변수의 변화를 본 연구는 제외하였다.
- 위의 검색엔진과 검색식을 통하여 국외 데이터베이스인 PUBMED에서 1,732건, EMBASE에서 1,032건, CINAHL에서 67건, PsycINFO에서 156건이 검색되었으며, 국내 데이터베이스인 학술연구정보서비스(RISS)에서 7건이 검색되어 총 2,994건의 문헌이 검색되었다. ENDNOTE를 활용하여 중복된 문헌 322건을 제거하였으며, 제목과 초록을 통해 선정기준에 맞지 않는 2,619건을 제거하였다. 53건의 문헌의 전문을 살펴보아 문헌의 적합성을 검증하였고 이 중 9건의 문헌이 연구대상으로 인해, 23건이 연구 디자인으로, 5건이 결과변수로, 3건이 초록만 포함하는 등 문헌의 전문을 포함하지 않아 제거되었으며 최종적으로 총
- 13건의 문헌이 선정되었다(Fig. 1).
- 3. 자료분석
- 최종 13편의 문헌[9,14-24,29]의 특성을 반복 확인하여 분석과 평가에 필요한 자료가 누락되지 않도록 검토하였다. 각 문헌의 특성과 효과를 파악하기 위하여 프로그램의 목표, 이론적 근거, 참여자, 구성요소, 측정방법, 변수, 그리고 효과에 대해 분석을 실시하였다.
- 4. 문헌평가
- 최종 선정된 문헌의 질 평가는 Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2)를 바탕으로 진행하였다. 이 도구의 평가 항목은 다섯 가지 도메인인 ‘무작위 배정 절차(Randomization process)’, ‘의도한 중재로부터의 벗어남(Deviations from intended intervention)’, ‘불완전한 결과의 처리(Missing outcome data)’, ‘결과의 측정(Measurement of the outcome)’, ‘선택적 결과보고(Selection of the reported result)’로 구성되어 있다. 각 도메인의 세부 문항은 ‘그렇다(Yes)/아마도 그렇다(Probably Yes)/아니다(No)/ 아마도 그렇지 않다(Probably No)/정보 없음(No Information)’의 다섯 가지로 응답할 수 있다. 최종적인 질 평가로 Low Risk, Some concerns, High risk 중 한 가지로 판단할 수 있다. 두 연구자가 각자의 공간에서 독립적으로 도구의 기준에 따라 질 평가를 시행하였다. 연구자간 응답이 불일치한 경우 해당 문헌을 함께 살펴본 후 놓친 정보는 없는지 등의 재평가 논의를 통해 최종적인 질 평가를 완료하였다.
연구방법
1) 문헌 검색 전략
2) 핵심 질문
3) 데이터베이스 및 검색어
4) 문헌 선정 및 제외 기준
5) 문헌선택과정
- 1. 문헌의 일반적 특성
- 의사소통 중재 프로그램을 시행한 13편 문헌[9,14-24,29]에 대한 일반적 특성은 Table 1과 같다. 2011년에서 2015년 사이에 출판된 문헌은 9편[9,14-20,29]이었다. 연구 수행 국가를 살펴보면 미국이 4편[14,16,22,24]으로 가장 많았고 네덜란드[15,20], 이란[17,23], 대만[19,29]에서 시행한 연구가 각 2편이었다. 연구 참여자들은 다양한 부서에서 근무하고 있었으나 수술실과 정신과 부서에서 근무하는 간호사 대상의 연구는 없었다. 연구 참여자의 평균 연령이 20세 이상 30세 미만인 문헌이 4편[9,19,23,29]으로 가장 많았고, 연구 참여자의 수는 40명 이상 80명 미만이 5편[14,15,17,21,22]으로 가장 많았다.
- 2. 문헌의 질 평가
- 다섯 가지 도메인인 ‘무작위 배정 절차’, ‘의도한 중재로부터의 벗어남’, ‘불완전한 결과의 처리’, ‘결과의 측정’, ‘선택적 결과보고’를 기반으로 하여 13건의 문헌의 질 평가를 시행하였다. 다섯 가지 도메인 모두에서 Low risk 판단을 받아야 전반적인(Overall) 질 평가에서 Low risk의 평가를 받을 수 있다. 최소 하나 이상의 도메인에서 Some concerns 판단을 받으면 전반적인 질 평가에서 Some concerns의 평가를 받게 되고, 최소 하나 이상의 도메인에서 High risk 판단을 받게 되면 전반적인 질 평가에서 High risk의 평가를 받는다.
- 최종적으로 질 평가를 시행한 결과를 살펴보면 Low risk 문헌은 3편[14,15,22], Some concerns 문헌은 8편[9,16, 18-21,23,29], High risk 문헌은 2편[17,24]으로 나타났다(Table 2). 도메인 2, 3, 5에서는 Low risk가 대부분을 차지하는 반면, 도메인 1과 도메인 4에서는 Some concerns 혹은 High risk의 문제가 발생하였다.
- 3. 병원 간호사 대상의 의사소통 프로그램 특성
- 각 문헌에서 제시한 참여자의 특성, 프로그램의 형식, 구체적인 중재방법, 측정방법, 결과변수 그리고 효과는 Table 3, 4와 같다.
- 13건의 문헌 중에서 간호사만 대상으로 한 문헌은 12편[9,14,15,17-24,29]이며, 간호사뿐 아니라 레지던트와 펠로우를 포함한 문헌은 1편[16]이었다. 신규 간호사만을 대상으로 한 연구는 1편[9]이 있었으며 신규 간호사를 일부 포함하여 진행한 연구는 2편[19,29]이 있었다.
- 13편 모두 대인관계 증진을 위한 연구였으며, 환자와의 관계 증진을 포함한 연구가 11편[9,14-20,23,24,29]으로 가장 많았다. 프로그램의 주요 개념을 살펴보면 어려운 상황에서의 의사소통[14], 통증 관리[16], 퇴원 계획[29], 공감[21], 자기 주장적 의사소통[22], 민감한 이슈를 다룰 때의 의사소통[24] 등으로 다양했다. 프로그램의 이론적 근거를 제시한 연구는 11편[9,14-16,18-23,29]으로 대부분의 연구에서 중재의 이론적 기틀을 제공하였다.
- 중재 회기는 1회기성의 워크샵부터 8회기까지 다양했으며, 8회기의 중재를 시행한 연구가 4편[9,16,19,23]로 가장 많았다. 중재를 시행한 총 시간은 3시간부터 105시간까지 다양하게 나타났으며, 중재를 제공하는 총 기간이 1달 이상 3달 미만인 연구는 7편[9,15,17,18,21-23]으로 가장 많았다.
- 중재 방법으로는 강의, 활동(Activity), 디브리핑, 과제를 활용하였으며, 모든 문헌에서 활동의 방법을 적용하였고 디브리핑을 활용한 연구는 11편[9,14-16,18-22,24, 29]이었다. 강의를 시행한 연구는 10편[9,14,16-20,22,24,29]이 있었으나 강의만 단독으로 시행한 연구는 없었다. 각 문헌에서 시행한 활동들을 구체적으로 살펴보면 서면 자료, 비디오/DVD/필름, 시뮬레이션, 반영, 온라인 매체 등이 있었고, 대부분의 연구에서 여러 활동들을 병행하여 중재를 제공하였다. 시뮬레이션은 가장 많이 사용된 방법으로 총 10편[9,14-16,18,19,21,22,24,29]의 문헌에서 사용되었으며, 반영을 적용한 연구는 8편[14-16,19-21, 23,29]이었다. 그러나 온라인 매체를 활용한 문헌은 3편[15,20,22]에 불과했다. 특히, 시뮬레이션의 수준이 역할극(role-play), 연극 기법 적용, 삽화, 사례, 시나리오 등으로 다양했으며 역할극을 사용한 연구가 6편[14-16,18, 21,22]으로 가장 많았다.
- 프로그램의 중재 효과를 측정하기 위한 측정 방법은 다음과 같다. 사전, 사후 총 2회 측정한 연구는 11편[9,14-18, 20-24]으로 가장 많았으며, 사전 측정을 포함하여 총 3회 측정한 연구는 2편[19,29]이었다.
- 프로그램의 효과를 측정하기 위하여 주관적•객관적 지표가 사용되었으며, 객관적 지표를 통한 측정은 총 10편의 연구에서 사용되었다. 구체적으로 살펴보면 객관적 지표만을 적용한 연구는 5편[15,18,20,22,24], 객관적•주관적 지표를 모두 적용한 연구는 5편[9,14,16,19,29]이었다. 객관적 지표를 활용한 연구 중 기존에 개발된 측정도구를 사용한 연구는 5편[14,19,20,22,29]으로, 이중 가장 많이 사용한 도구는 객관적-구조적 임상능력평가(Objective Structured Clinical Examination, OSCE)였다. 연구자가 개발한 객관적 지표를 활용한 연구는 5편[9,14,15,18, 24]이었는데 이 중에서 2편[15,18]의 경우 인터뷰 녹음 혹은 비디오 녹화 내용을 빈도 분석하였고, 1편[24]은 의사소통 행위에 대한 체크리스트를 활용하였고, 1편[9]은 실제 조기 사직률을 계산하는 등 측정의 범위와 대상이 다양했다. 객관적 지표를 사용하여 측정한 경우 관찰자 혹은 평가자 등이 간호사의 의사소통을 평가한 문헌은 7편[14,15,18-20,22,24]이었으며 표준화 환자가 간호사의 의사소통을 평가한 문헌은 1편[29]이었다.
- 대부분의 연구에서 최소 하나 이상의 유의한 의사소통 관련 변수가 있었으며, 가장 많이 측정된 변수는 의사소통기술과 의사소통행동이었고 그 외 측정된 변수로는 의사소통효능감, 의사소통유능감, 학습 만족도, 의사소통의 질, 환자의 우울, 직무 만족도, 자아존중감, 이직의도 등이 있었다. 구체적인 결과를 살펴보면 8편[15,17,18,20-24]이 의사소통기술에 초점을 맞추었으며 이중 4편[17,21,23,24]은 유의하였으며 3편[15,18,20]은 의사소통기술의 일부분만 유의하였다. 의사소통기술을 측정할 때 사용한 도구가 연구마다 제각각 달랐으며 특히, 연구자가 개발한 의사소통기술 도구를 사용한 경우 의사소통기술의 일부분만 유의한 것으로 나타났다[15,18,20]. 1편[15]의 경우 7가지 이슈 중에 2가지인 ‘Discussing realistic expectations’, ‘Less rehabilitation information’만 유의하였고, 1편[18]의 경우 12개의 의사소통 전략 중 ‘More questions about pain related emotion’, ‘Assess cognition with pain more frequently’, ‘Less paternalistic statement’가 유의했으며, 1편[20]의 경우 의사소통기술의 13개 척도 중 3개인 ‘request for help’, ‘physical examination’, ‘information giving’만 유의한 것으로 나타났다. 의사소통행위 증진에 목표를 둔 4편[14,19,24,29]의 경우 1편[24]이 유의했으며, 1편[29]의 경우 표준화 환자가 측정한 행동은 유의하지 않았으나 외부 평가자(instructors)가 평가한 행동만 부분적으로 유의했으며, 나머지 2편[14,19]의 경우 유의하지 않았다. 간호사의 의사소통행위를 측정하기 위해서 객관적-구조적 임상능력평가(OSCE)가 주로 사용되었다.
- 객관적, 주관적 지표에 따른 의사소통기술 및 의사소통행위 변수의 유의성 여부를 살펴보면 다음과 같다. 해당 변수를 객관적 지표를 통해 측정한 연구는 8편[14,15,18-20,22,24,29]이었으며 이중 3편[14,19,22]은 유의하지 않았고 4편[15,18,20,29]은 일부분만 유의한 것으로 나타났다. 반면, 주관적 지표를 활용한 연구는 3편[17,21,23] 이었고 모두 유의한 결과를 보였다.
결 과
1) 참여자의 특성
2) 프로그램의 내용과 형식
3) 측정 방법
4) 주요 변수와 효과
- 본 연구는 2011년부터 2020년까지 국내외에서 출판된 문헌 중 병원에서 근무하는 간호사를 대상으로 시행된 의사소통 프로그램의 특성과 효과를 체계적으로 고찰하고자 하였다. 최근 10년간의 의사소통 프로그램의 동향을 살펴본 후 간호사 대상의 효과적인 의사소통 중재의 전략과 방향에 대해 살펴보고자 한다.
- 선정 및 제외 기준에 부합한 13편의 문헌이 분석과정을 거쳤으며, 13편 모두 모두 무작위 대조군 사전-사후 연구였다. 그러나 무작위 배정 절차에 대해 언급이 없거나 부적절하게 시행되었고, 대상자의 기술 및 행동 변화를 관찰하는 중재연구 특성상 이중 눈가림이 진행되기 쉽지 않았다. 그로 인해 질 평가 시 도메인1에서 문제가 여러 문헌에 드러났으며 이러한 편향(bias)이 도메인4인 측정에까지 영향을 미치는 것으로 나타났다. 도메인1과 4에서의 편향을 줄이기 위해서는 무작위 배정을 연구와 무관한 제3자가 시행하고, 참여자의 행동을 측정할 경우 중재 진행과 관계없는 관찰자가 평가해야 할 것이다. 또한, 연구설계의 근거, 한계점 등을 포함하여 연구 진행과정에 대해 상세히 언급하는 것이 필요하다.
- 연구 참여자가 근무하는 부서가 매우 다양했으나 수술실과 정신과에서 근무하는 간호사는 없었다. 수술실 간호사의 경우 폐쇄된 공간에서 수술 진행과 관련된 간단한 의사소통만 하므로 의사소통의 중요성에 대한 인식이 낮았을 것이며[30], 자신을 치료적 도구로 활용하는 정신간호사의 특성상 의사소통역량이 일반병동 간호사보다 높으므로 의사소통 교육에 대한 필요성이 낮아 이들을 위한 연구가 없었을 것이다[31]. 실제로 수술실 간호사의 경우 병동 간호사보다 의사소통역량이 더 낮았고 위계화된 의사소통, 소극적인 자기주장 그리고 불명확한 의사소통을 경험하는 것으로 나타나 수술실 간호사를 위한 의사소통 교육이 요구된다[30,32]. 최근 정신간호사와 대상자의 치료적 관계 및 상호작용이 감소하고 있다는 보고가 있으므로 정신간호사를 대상으로 지속적인 치료적 의사소통기술 훈련이 필요하다[33]. 따라서 향후 간호사 대상의 의사소통 교육 중재를 제공할 때 일반병동, 특수병동 등의 다양한 부서 각각의 의사소통 특성과 요구를 고려하여 임상현장에서 적용 가능한 맞춤형의 중재를 제공해야 한다.
- 신규 간호사를 포함한 문헌은 3편이었는데, 이중 연차에 따라 차별화된 교육을 제공한 문헌은 1편이었고 나머지 2편의 경우 경력 여부와 관계없이 같은 교육을 제공하였다. 신규 간호사의 의사소통 경험을 살펴보면 동료 간호사, 의사, 환자로부터 무시를 당하거나 태움과 폭언과 같은 대인관계의 문제를 많이 경험하는 것으로 나타났으며, 이러한 문제가 반복적으로 발생하면 결국 이직을 고려했다[34]. 이를 반영하듯 신규 간호사의 이직률은 42.7%로 평균 간호사의 이직률인 15.7%보다 무려 2.7배 더 높은 것으로 나타났다[35]. 한편, 경력이 증가하면서 의사소통기술은 향상되나 위중한 환자 관련 업무를 맡게 되는 등 더 많은 책임을 가지게 되므로 신규 간호사와는 다른 의사소통 상황을 직면하게 될 것이다. 따라서 간호사의 경력에 따라 경험하는 의사소통 문제들을 탐색한 후 이에 대한 프로그램을 개발하고 제공하는 것이 필요하겠다.
- 본 연구에서 분석한 문헌들을 살펴보면 주로 간호사-환자의 관계 증진 연구가 주를 이루고 있었으며 의료진간의 의사소통을 다루고 있는 문헌은 3편에 불과했다. 의료사고의 60∼70%가 의료진간의 의사소통문제로 기인한다는 통계자료[36]를 감안했을 때 의료진 간의 의사소통을 위한 프로그램도 활발하게 이루어져야 한다. 특히, 간호사와 의사간의 의사소통문제는 환자의 부정적인 건강결과나 안전사고로 이어지기 때문에 상호존중을 기반으로 한 정확한 의사소통이 필수적이다. 또한, 지금까지 공감, 자기주장, 퇴원계획, 민감한 이슈를 다루는 등의 다양한 개념을 기반으로 하여 의사소통 프로그램을 개발한 것으로 나타났다. 앞으로 각 부서에서 발생하는 여러 임상현장에 맞게 임종간호, 노인 혹은 아동 환자와의 의사소통 등의 더욱 다양한 개념을 활용하여 프로그램을 개발하는 것이 필요하다.
- 중재 프로그램마다 중재 회기/시간/기간이 상이했으며, 가장 많은 문헌에서 보고한 중재 회기는 8회기였고 중재 기간은 1달 이상 3달 미만이었다. 간호대학생들을 대상으로 의사소통 프로그램의 효과를 메타분석한 연구[1]에 따르면 의사소통 기술은 단기간에 증진되는 것이 아니므로 단 회기성의 교육보다 지속적인 훈련과 학습을 강조하였다. 또한, 의사소통 프로그램을 메타분석 한 연구[37]에 따르면 9∼10회기, 70∼150분의 시간, 총 5∼8주의 기간을 포함한 프로그램이 효과 크기가 가장 크다고 보고했다. 선행연구들[1,37]의 결과를 고려하여 추후 간호사 대상의 의사소통 프로그램의 중재 회기/시간/기간을 결정해야 할 것이다.
- 분석에 포함된 연구들의 경우, 의사소통 프로그램을 시행할 때 강의만 단독으로 시행하기보다 시뮬레이션, 온라인 매체의 활용, 과제 등의 여러 방법을 병용한 것으로 나타났으며, 그중 역할극을 활용한 시뮬레이션 교육과 디브리핑이 가장 활발하게 이루어졌다. 간호사를 대상으로 한 시뮬레이션의 교육 효과는 큰 편이었으며[38], 역할극을 활용하였을 때 대인관계능력, 의사소통기술, 문제해결능력 그리고 자기효능감이 통계적으로 유의하게 상승한다고 보고했다[39]. 디브리핑을 제공할 때는 강의식 방법은 지양하고 자신의 수행을 직접 관찰한 후 피드백을 받는 방법이 효율적이다[40]. 앞으로도 간호교육에 시뮬레이션과 자아성찰을 기반으로 한 디브리핑 방법을 통해 간호사들의 의사소통역량을 강화하는 것이 필요하겠다.
- 웹 기반 기술이 다양한 분야에서 활용되고 있는 추세와는 달리 본 연구에 포함된 문헌들을 살펴보면 웹 기반의 연구는 3편에 불과했다. 간호사와 간호학생을 대상으로 가상현실을 활용한 프로그램의 동향을 조사한 연구[41]에 따르면 2013년이 되어서야 본격적으로 해당 연구가 시행되었기에 관련 문헌이 적었을 것으로 판단된다. 그러나 가상현실을 포함한 웹 기반 기술이 교육, 운동 등의 다양한 영역에서 활용되고 있으며, COVID-19 팬데믹으로 인해 비대면 실습교육의 중요성과 필요성이 대두되고 있는 상황을 고려했을 때 앞으로 온라인 매체를 활용한 프로그램이 더욱 활발히 개발될 것으로 예상된다. 간호교육을 위해 시행된 웹 기반 시뮬레이션의 연구동향을 살펴보면 특정 간호술기를 교육하거나 심폐소생술과 같이 시행순서를 습득하는 시뮬레이션이 주를 이루었으며, 의사소통과 같이 상황적 시뮬레이션을 다루는 연구는 적은 비중을 차지했다[42]. 향후 간호사를 대상으로 온라인 매체를 기반으로 한 의사소통 시뮬레이션 프로그램을 개발하고 그 효과를 평가하는 것이 필요하다.
- 본 연구에 포함된 중재 프로그램의 측정방법을 살펴보면 주관적 지표를 활용한 연구는 3편에 불과했고, 10편에서 객관적 지표를 사용하고 있음을 알 수 있다. 연구자가 개발한 객관적 지표를 사용한 문헌은 5편이었으며, 각 연구마다 항암병동, 신생아 중환자실 등과 같이 특정 임상현장에 맞추었기 때문에 평가기준이 문헌마다 상이했다. 객관적 지표인 객관적-구조적 임상능력평가(OSCE)를 사용하여 간호사의 의사소통행동을 측정한 연구[29]에서 외부 평가자가 측정한 간호사의 의사소통행동 변화는 유의하였고 동일한 간호사를 대상으로 표준화 환자가 측정한 경우 유의하지 않았던 점은 주목할 만하다. 향후 연구에서는 평정자간 신뢰도(inter-rater reliability)를 확인하는 것이 필요하고, 잘 훈련되고 적절한 자격을 갖춘 평가자들이 간호사들의 의사소통기술 및 행동을 측정할 수 있도록 평가자들의 질을 관리하는 것이 요구된다. 본 연구에서 의사소통역량을 측정하기 위해 객관적 지표를 많이 사용한 것은 고무적이지만, 연구자가 개발한 지표나 주관적 보고에 따른 지표들을 사용한 연구가 많아서 중재의 효과를 상호비교하기 어려웠다. 더욱이, 같은 객관적-구조적 임상능력평가(OSCE) 도구를 사용했더라도 평가자에 따라 중재의 효과가 다르게 나타나 상호비교가 더욱 쉽지 않았다. 임상현장의 상황별 특성을 다각도로 고려한 도구의 개발도 필요하지만, 전반적인 의사소통역량을 일괄된 지표로 측정할 수 있는 도구를 개발하는 것 역시 필요하겠다.
- 프로그램의 대상자, 내용 및 구성방식 등이 다양했으나 본 연구에 포함된 문헌의 대부분이 간호사의 의사소통역량을 향상시키는 것으로 나타났다. 가장 많이 측정된 변수는 의사소통기술과 의사소통행동이었고, 이를 주관적 지표를 통해 측정한 경우 3편 모두 유의했으나 객관적 지표를 활용하여 측정을 한 경우 8편 중 3편은 유의하지 않았고 4편이 변수의 일부만 유의한 것으로 나타났다. 도구의 상이함도 있겠지만 주관적 보고에 따라 중재의 효과를 평가한 경우 실제 의사소통기술 및 의사소통행동 수준과는 다르게 측정의 정확도가 떨어질 수 있다[43]. 또한, 자가보고에 따른 의사소통역량의 향상이 학습 만족도와 관련성이 있으나 실제 의사소통행동과는 상관관계가 없다고 보고한 연구[44]도 있으므로 간호사 대상으로 의사소통 중재의 효과를 측정할 때는 연구의 목적 등을 고려하여 주관적 혹은 객관적 지표의 사용을 고려해보는 것이 좋겠다. 특히, 중재연구의 특성상 프로토콜을 기반으로 하여 중재를 제공하는 것이 중요한데 본 연구에서 프로토콜 기반의 중재를 제공한 문헌은 일부[15,23,29]에 불과했다. 구체적인 절차를 포함한 근거 기반의 프로그램을 진행하여 연구의 타당성을 확보하고 동일한 중재를 다양한 대상자에게 적용하기 위해서 프로토콜 기반의 연구가 요구된다.
- 본 연구에 포함된 13편 문헌에서 시행된 프로그램의 목적은 모두 병원에서 근무하는 간호사의 의사소통역량 향상을 위해 진행되었다. 그러나 프로그램의 효과를 통합적으로 비교 및 분석하기에는 어려움이 있었는데 그 이유는 프로그램의 이론적 기틀, 중재 기간, 측정방법, 중재 구성요소가 제각각이었고, 측정도구가 다양하여 측정의 범위와 대상이 상이했기 때문이다. 하지만 각자 다른 중재의 특성과 측정 도구에도 불구하고 분석에 포함된 대부분의 연구에서 중재 적용 결과 의사소통 관련 변수의 향상이 있었다는 것은 큰 의미를 갖는다. 이를 바탕으로 향후 간호사들을 대상으로 의사소통 중재 프로그램을 개발하여 간호사들의 의사소통역량을 향상시키고자 한다.
- 본 연구의 제한점은 다음과 같다. 영어와 한국어로 작성된 문헌만을 포함했다는 점이다. 그럼에도 불구하고 본 연구는 최근 10년간 국내외의 병원에서 근무하는 간호사를 대상으로 시행한 의사소통 프로그램의 특성, 효과 및 동향을 파악하고 앞으로의 의사소통 교육의 방향성을 제시했다는 점에서 의의가 있다.
고 찰
-
Conflicts of Interest
The authors declared no conflict of interest.
-
Funding
This research was supported by the BK21 four project (Center for Human-Caring Nurse Leaders for the Future) funded by the Ministry of Education (MOE, Korea) and National Research Foundation of Korea (NRF).
Notes
- 1. Han MW, Lee KH. 2017;Effects of communication ability enhancement program for nursing students in Korea: A systematic review and meta-analysis. The Journal of Korean Academic Society of Nursing Education. 23(1):15-26. doi: 10.5977/jkasne.2017.23.1.15.Article
- 2. Kim HJ. 2017;Evaluation of motivational interviewing training to promote client-centered communication competency for nurses. Journal of Korean Academy of Psychiatric and Mental Health Nursing. 26(4):362-373. doi: 10.12934/jkpmhn.2017.26.4.362.Article
- 3. Garon M. 2012;Speaking up, being heard: Registered nurses' perceptions of workplace communication. Journal of Nursing Management. 20(3):361-371. doi: 10.1111/j.1365-2834.2011.01296.x.ArticlePubMed
- 4. Kang MJ, Lee HJ. 2003;A phenomenological study on nurses' experiences of turnover. Journal of Korean Academy of Nursing Administration. 9(3):305-314.
- 5. Cho YA, Kim KS. 2013;Effects of assertiveness training for ICU nurses. Journal of Korean Clinical Nursing Research. 19(2):255-264. doi: 10.22650/JKCNR.2013.19.2.255
- 6. Bae SH, Park JS. 2015;Development and evaluation of extracurricular coaching programs for improving communication skills and leadership among nursing students. Journal of Korean Academic Society of Nursing Education. 21(2):202-214. doi: 10.5977/kasne.2015.21.2.202.Article
- 7. Shin YH, Lee S, Moon HS, Jung , DY , Lee HS. 2018;Effects of Satir's model based communication education on communication competence, emotional intelligence and depression-happiness of regional public hospital nurses. Journal of Korean Public Health Nursing. 32(1):122-134. doi: 10.5932/JKPHN.2018.32.1.122
- 8. Shin NY. 2018;The effect of simulation-based training applying Situation-Background -Assessment-Recommendation (SBAR) on nurse shift handover on self efficacy and communication skills in new nurses. Journal of Korean Society for Simulation in Nursing. 6(2):57-68. doi: 10.17333/JKSSN.2018.6.2.57.Article
- 9. Koo MJ, Kim KN. 2012;A study on the development and evaluation of hospital communication (hospital adaptation) program for new graduate nurses. The Korean Journal of Health Service Management. 8(4):1-12. doi: 10.12811/kshsm.2014.8.4.001.Article
- 10. Shin JA, Cho YA. 2020;The development and effects of communication improvement education program for nurses and physicians in nursing care integrated service ward. Korean Public Health Research. 46(1):17-31. doi: 10.22900/kphr.2020.46.1.002
- 11. Kim KI, Kim SJ, Kim BY. 2018;A convergence study about the effects of assertiveness training on nurses' fear of negative evaluation, assertiveness behavior, and communication competency. Journal of the Korea Convergence Society. 9(10):487-495. doi: 10.15207/JKCS.2018.9.10.487
- 12. Kim YH, Choi YS, Jun HY, Kim MJ. 2016;Effects of SBAR program on communication clarity, clinical competence and self-efficacy for nurses in cancer hospitals. The Korean Journal of Rehabilitation Nursing. 19(1):20-29. doi: 10.7587/kjrehn.2016.20.Article
- 13. Lee MO, Lee SB. 2016;Effects of nonviolent communication program consist of communication ability, relationship and anger in nurses. Journal of the Korea Society of Computer and Information. 21(10):85-89. doi: 10.9708/jksci.2016.21.10.085.Article
- 14. Doyle D, Copeland HL, Bush D, Stein L, Thompson S. 2011;A course for nurses to handle difficult communication situations: A randomized controlled trial of impact on self-efficacy and performance. Patient Education and Counseling. 82(1):100-109. doi: 10.1016/j.pec.2010.02.013.ArticlePubMed
- 15. Van Weert JC, Jansen J, Spreeuwenberg PM, van Dulmen S, Bensing JM. 2011;Effects of communication skills training and a question prompt sheet to improve communication with older cancer patients: A randomized controlled trial. Critical Reviews in Oncology/hematology. 80(1):145-159. doi: 10.1016/j.critrevonc.2010.10.010.ArticlePubMed
- 16. Curtis JR, Back AL, Ford DW, Downey L, Shannon SE, Doorenbos AZ, et al. 2013;Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: A randomized trial. Jama. 310(21):2271-2281. doi: 10.1001/jama.2013.282081.ArticlePubMedPMC
- 17. Khodadadi E, Ebrahimi H, Moghaddasian S, Babapour J. 2013;The effect of communication skills training on quality of care, self-efficacy, job satisfaction and communication skills rate of nurses in hospitals of Tabriz, Iran. Journal of Caring Sciences. 2(1):27-37. doi: 10.5681/jcs.2013.004PubMedPMC
- 18. Canivet D, Delvaux N, Gibon AS, Brancart C, Slachmuylder JL, Razavi D. 2014;Improving communication in cancer pain management nursing: A randomized controlled study assessing the efficacy of a communication skills training program. Supportive Care in Cancer. 22(12):3311-3320. doi: 10.1007/s00520-014-2357-2.ArticlePubMed
- 19. Hsu LL, Huang YH, Hsieh SI. 2014;The effects of scenario-based communication training on nurses' communication competence and self-efficacy and myocardial infarction knowledge. Patient Education and Counseling. 95(3):356-364. doi: 10.1016/j.pec.2014.03.010.ArticlePubMed
- 20. Noordman J, van der Weijden T, van Dulmen S. 2014;Effects of video‐feedback on the communication, clinical competence and motivational interviewing skills of practice nurses: A pre‐test posttest control group study. Journal of Advanced Nursing. 70(10):2272-2283. doi: 10.1111/jan.12376.ArticlePubMed
- 21. Kahriman I, Nural N, Arslan U, Topbas M, Can G, Kasim S. 2016;The effect of empathy training on the empathic skills of nurses. Iranian Red Crescent Medical Journal. 18(6):e24847. doi: 10.5812/ircmj.24847.ArticlePubMedPMC
- 22. Oner C, Fisher N, Atallah F, Son MA, Homel P, Mykhalchenko K, et al. 2018;Simulation-based education to train learners to "speak up" in the clinical environment: Results of a randomized trial. Simulation in Healthcare. 13(6):404-412. doi: 10.1097/SIH.0000000000000335.ArticlePubMed
- 23. Pangh B, Jouybari L, Vakili MA, Sanagoo A, Torik A. 2019;The effect of reflection on nurse-patient communication skills in emergency medical centers. Journal of Caring Sciences. 8(2):75-81. doi: 10.15171/jcs.2019.011.ArticlePubMedPMC
- 24. Bowen R, Lally KM, Pingitore FR, Tucker R, McGowan EC, Lechner BE. 2020;A simulation based difficult conversations intervention for neonatal intensive care unit nurse practitioners: A randomized controlled trial. PloS one. 15(3):e0229895. doi: 10.1371/journal.pone.0229895.ArticlePubMedPMC
- 25. Omura M, Maguire J, Levett-Jones T, Stone TE. 2017;The effectiveness of assertiveness communication training programs for healthcare professionals and students: A systematic review. International Journal of Nursing Studies. 76:120-128. doi: 10.1016/j.ijnurstu.2017.09.001.ArticlePubMed
- 26. Muller M, Jurgens J, Redaelli M, Klingberg K, Hautz WE, Stock S. 2018;Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ open. 8(8):e022202. doi: 10.1136/bmjopen-2018-022202.ArticlePubMedPMC
- 27. Kerr D, Ostaszkiewicz J, Dunning T, Martin P. 2020;The effectiveness of training interventions on nurses' communication skills: A systematic review. Nurse Education Today. 89:104405doi: 10.1016/j.nedt.2020.104405.ArticlePubMed
- 28. Kim SY, Park JE, Seo HJ, Lee YJ, Jang BH, Son HJ, et al. 2011, NECA's guidance for undertaking systematic reviews and meta-analyses for intervention. National Evidence-based Healthcare Collaborating Agency; Seoul.
- 29. Hsu LL, Chang WH, Hsieh SI. 2015;The effects of scenario-based simulation course training on nurses' communication competence and self-efficacy: A randomized controlled trial. Journal of Professional Nursing. 31(1):37-49. doi: 10.1016/j.profnurs.2014.05.007.ArticlePubMed
- 30. Lim EJ, Yi YJ. 2014;Comparison of operating room nurses and general ward nurses on communicative competence and interpersonal relationship ability within the medical team. Korean Academy of Nursing Administration. 20(3):313-321. doi: 10.11111/jkana.2014.20.3.313.Article
- 31. Son MR, Kim SH. 2020;The mediating effect of empowerment on the relationship between communication ability and nursing performance in psychiatric nurses. The Korean Academy of Psychiatric and Mental Health Nursing. 29(2):177-184. doi: 10.12934/jkpmhn.2020.29.2.177.Article
- 32. Ahn SA, Lee NJ. 2019;Experience of communication for patient safety by perioperative nurses. Korean Academy of Nursing Administration. 25(4):329-339. doi: 10.11111/jkana.2019.25.4.329.Article
- 33. Cleary M, Hunt GE, Horsfall J, Deacon M. 2012;Nurse-patient interaction in acute adult inpatient mental health units: A review and synthesis of qualitative studies. Issues in Mental Health Nursing. 33(2):66-79. doi: 10.3109/01612840.2011.622428.ArticlePubMed
- 34. Kim CS. 2020;Communication experience of new nurses in some general hospitals. Health Service Management Review. 14(1):1-12. doi: 10.18014/hsmr.2020.14.1.01.
- 35. Hospital Nurses Association. 2019, Business report for hospital nurses association 2018. Hospital Nurses Association; Seoul.
- 36. The Joint Commission. 2017, High reliability healthcare: The art of hand-off communication. The Joint Commission; Oakbrook Terrace, Illinois.
- 37. Park EH. 2014;Daegu: Kyunpook National University; 2014. Kyunpook National University; Daegu.
- 38. Kim SH, Ham YS. 2015;A meta-analysis of the effect of simulation based education: Korean nurses and nursing students. The Journal of Korean Academic Society of Nursing Education. 21(3):308-319. doi: 10.5977/jkasne.2015.21.3.308.Article
- 39. Seo YA, Yoon SH, Kim YA. 2019;The effects of domestic nursing practical education using role-play: A systematic review and meta-analysis. The Korean Data and Information Science Society. 30(2):309-321. doi: 10.7465/jkdi.2019.30.2.309.Article
- 40. Kim EJ, Kim YJ, Moon SM. 2017;Nursing students' perceptions of meaning, response, and effective methods for debriefing in simulation-based education. Journal of Korean Academy of Fundamentals of Nursing. 24(1):51-59. doi: 10.7739/jkafn.2017.24.1.51.Article
- 41. Kim SK, Eom MR, Park MH. 2019;Effects of nursing education using virtual reality: A systematic review. Journal of the Korea Contents Association. 19(2):661-670. doi: 10.5392/JKCA.2019.19.02.661
- 42. Cant RP, Cooper SJ. 2014;Simulation in the internet age: The place of web-based simulation in nursing education. An integrative review. Nurse Education Today. 34(12):1435-1442. doi: 10.1016/j.nedt.2014.08.001.ArticlePubMed
- 43. Muckler FA, Seven SA. 1992;Selecting performance measures: "Objective" versus "subjective" measurement. Human Factors. 34(4):441-455. doi: 10.1177/001872089203400406.Article
- 44. Mullan BA, Kothe EJ. 2010;Evaluating a nursing communication skills training course: The relationships between self-rated ability, satisfaction, and actual performance. Nurse Education in Practice. 10(6):374-378. doi: 10.1016/j.nepr.2010.05.007.ArticlePubMed
References
Figure & Data
References
Citations

- A Survey on Situation-related Communication Educational Needs for Novice Intensive Care Unit Nurses
Wonjung Hwang, Jeongmin Ha, Dahye Park
Journal of Korean Critical Care Nursing.2024; 17(1): 17. CrossRef - Technology-based interactive communication simulation for Korean nurses: A randomized controlled repeated-measures design
Heeseung Choi, Yeseul Jeon, Ujin Lee, Junggeun Ahn, Hannah Kim
Nurse Education Today.2023; 128: 105879. CrossRef - Non-Contact Nursing Education in Communication and Group Counseling: Current Status and Future Directions
Kuem Sun Han, Soo Yeon Lee, Ji Hye Shin
STRESS.2023; 31(4): 149. CrossRef
 PubReader
PubReader-
 Cite
Cite
- CITE
-
- Close
- Download Citation
- Close
 XML Download
XML Download
- Figure
- Related articles
-
- An Integrative Review of Psychosocial Intervention Programs for Infertile Females
- An Integrative Review on Heart Health Promotion Programs for Female Workers
- An Integrative Review of Simulation Programs for Nursing Students: Patient and Caregiver-Centered Communication
- An Integrative Review of Facial Emotion Information Processing in Depression