Articles
- Page Path
- HOME > STRESS > Volume 29(3); 2021 > Article
-
Original Articles
정신증 고위험군에 영향을 미치는 요인 -
장영은
 , 한금선
, 한금선
- Factors Affecting Clinical High Risk for Psychosis
-
Young Eun Jang
 , Kuem Sun Han
, Kuem Sun Han
-
stress 2021;29(3):158-167.
DOI: https://doi.org/10.17547/kjsr.2021.29.3.158
Published online: September 30, 2021
1삼육보건대학교 간호학과 조교수
2고려대학교 간호대학 교수
1Assistant Professor, Department of Nursing, Sahmyook Health University, Seoul, Korea
2Professor, College of Nursing, Korea University, Seoul, Korea
- Corresponding author, Kuem Sun Han, Tel: +82-2-3290-4919, Fax: +82-2-928-9108, E-mail: hksun@korea.ac.kr
• Received: May 29, 2021 • Revised: August 30, 2021 • Accepted: September 5, 2021
Copyright © 2021 by stress. All rights reserved.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,466 Views
- 45 Download
Abstract
-
Background
- For early detection of schizophrenia, we investigated the factors influencing young adults at clinical high risk (CHR) of psychosis and explained the structural model based on the Adolescent Resilience Model and the Stress Vulnerability Model.
-
Methods
- Based on web-based questionnaires, we measured perceived stress, family adaptability and cohesion, social support, coping, resilience, social function, and CHR in 907 cases.
-
Results
- Among 907 subjects, 102 (11.3%) were classified as CHR, and there was no difference according to demographic variables. Influencing factors of CHR were perceived stress, resilience, and social function. In the modified model, perceived stress, family adaptability and cohesion, and social support demonstrated a significant effect on coping. Perceived stress, family adaptability, cohesion, and coping demonstrated a significant influence on resilience. Perceived stress, coping, resilience, and social function demonstrated a significant influence on CHR.
-
Conclusions
- We suggest future research on the early stages of adolescence, and research that includes face-to-face surveys. Moreover, we recommend the development and selection of tools that can explain each influencing factor more lucidly.
- Recently, as an attempt to protect the human rights of the mentally ill, long-term hospitalization has been restricted, and thus, the issue of schizo-phrenia has become more concerning [1]. Groups with characteristic prodromal symptoms are termed as “clinical-high risk for psychosis” (CHR), or “early psychosis”, which is used inappropriately [2]. CHR indicates a group with a high risk of progressing to schizophrenia without any psychotic symptoms, whereas early psychosis indicates a state before diagnosis as schizophrenia with psychosis-sus-picious symptoms [3]. Clinically, “CHR”, “ultra-high risk” (UHR), “attenuated psychosis syndrome (APS)”, “early psychosis”, and “prodrome” are used concur-rently without any consideration. Although there is a difference in the timing of diagnosis, they all signify similar groups. However, as prodrome is a conceptually retrospective term, the term CHR is the most commonly used to emphasize that subjects with risk symptoms are to be detected and treated early [4].
- Schizophrenia can start in adolescence or early adulthood, and after several years of transition period, it develops into psychosis [5]. Despite gradual progression, the symptoms may go unnoticed [6]. Although early adulthood is one of the most psychologically vulnerable times, one experiences various challenges and actively adapts to social life as a part of human developmental, and it is the most critical period in the formation of personality [7]. However, if schizophrenia occurs at such time, it causes not only mental agony, but also issues in life in general. Negative experiences at this stage can worsen social dysfunction and impede recovery [8].
- According to Zubin and Spring, who conceptualized and proposed influencing factors affecting schizo-phrenia with regard to psychological, social, and biological factors, the expression of most schizo-phrenia is due to three factors: stress, protective factors, and individual buffering mechanisms [9]. In other words, excessive stress heightens the risk of transitioning to schizophrenia, and protective mechanisms that can protect an individual can diminish the influence of stress and the buffering mechanism prevents its transition [10]. This buffering mechanism hypothesis is innate and can be explained by genetics, individual characteris-tics, and healing power. Many studies claim that the risk of transitioning to schizophrenia increases when the buffering mechanism fails [11]. Many previous studies have reported social dysfunction immediately before the onset of schizophrenia, and such dysfunction has been proposed as a preceding factor of schizophrenia [12]. It has also been recognized that the CHR group has debili-tated social function, and social dysfunction is consi-dered important as a predictive factor for the diagnosis of CHR [13].
- Prodromal symptoms of schizophrenia are diverse and nonspecific, such as sleep disorder, depre-ssion, anxiety, and impaired interpersonal relations, which makes them prone to being overlooked and difficult to detect at an early stage due to variable progression [14]. Furthermore, the more delayed the diagnosis of schizophrenia, the more difficult its treatment becomes and prone to be chronic, causing various disorders such as deserted personality and social dysfunction. Thus, it creates a serious psychological and social burden not only on the patients but also their family [15]. Therefore, it is crucial to diagnose schizophrenia early and prevent it, but the fact that its negative and positive symptoms coexist makes it difficult for non-experts to discern CHR. Furthermore, even if the symptoms develop, patients rarely visit profe-ssional care centers as they fear social branding, which further hinders the chance of early diag-nosis [16].
- Research to prevent transition of the disease with prediction of schizophrenia and early inter-vention has become more active since the 90s, and multidisciplinary research to minimize the dura-tion of untreated psychosis (DUP) has achieved some positive feats, including shorter DUP [17]. However, imprudent early diagnosis and interven-tion strategies can also induce new problems, such as an increase in false positives, use of unnece-ssary psychotic medication, and social branding; therefore, an early diagnosis system based on reaso-nable selection criteria is necessary [18]. As those suffering CHR have 2∼3 times higher risk of schizo-phrenia than the general population, it is crucial to screen CHR amongst the general population for effective early diagnosis [19]. However, research to date is mostly clinic-based studies that must be diagnosed by psychiatrists [2,20,21], and most have been retrospective with outpatients or inpatients as their subjects, lacking prospective studies to screen CHR in the early stage with the general popula-tion as their subjects before the symptoms develop. In addition, although various factors have been investigated, comprehensive understanding has been insufficient and the age group of the subjects has been too broad, ranging from 12 to 45, making it difficult to find studies focused on early adulthood. Based on previous research, the current study provides a multidimensional review of the factors that may influence CHR with structural model verification of CHR in early adulthood screened from the general population.
- 1. Purpose
- This study sought to confirm the factors that may influence CHR in young adults. A hypothetical model that may explain the correlation between influential factors is constructed and model fit is verified. The specific goals are as follows:
- 1) Identify demographic characteristics of CHR.
- 2) Determine factors influential to CHR and set a hypothetical model based on preceding studies such as adolescent resilience and stress vulnerability models.
- 3) Propose a revised model for influential factors for CHR with fit evaluation between the hypothe-tical model and real data.
- 4) Verify the hypothesis on influential factors for CHR based on the revised model.
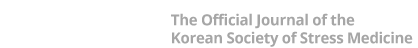
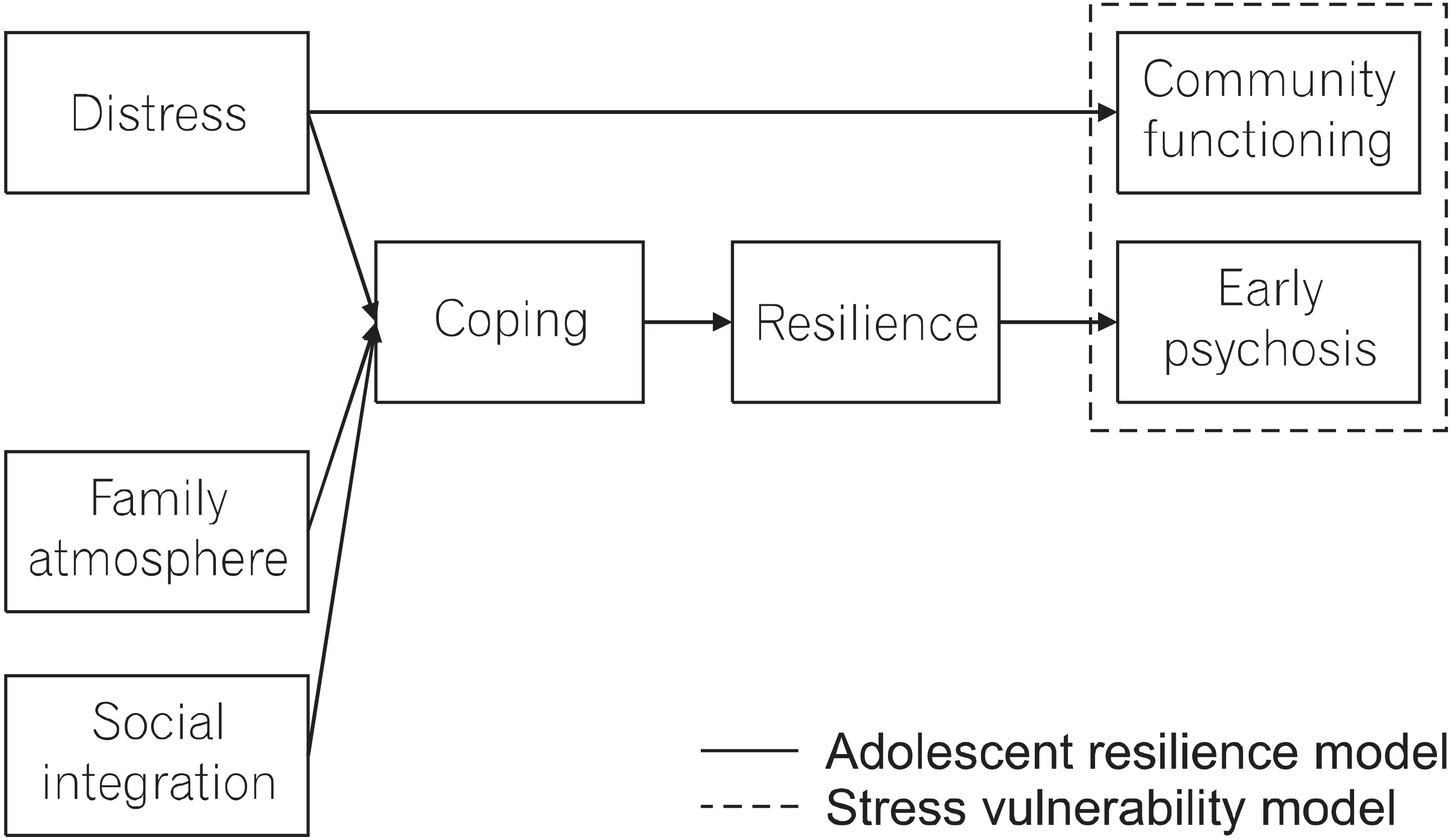
- 2. Theoretical framework and hypothetical model
- A theoretical framework was established by incorporating social function into the adolescent resilience model (ARM), based on the stress vulne-rability model (SVM) and preexisting literature to con-firm factors that may influence CHR [9,22]. Biological vulnerability, a key element of the stress vulnerability model, was difficult to evaluate using the survey method; therefore, it was replaced with resilience, a protective factor of the resilience model. A total of seven concepts of distress, family atmo-sphere, social integration, coping, resilience, com-munity functioning, and early psychosis were selected. Based on the theoretical framework, the hypoth-etical model has three exogenous variables (per-ceived stress, family adaptability and cohesion, and social support) and four endogenous variables (coping, resilience, social function, and CHR). This study established a research hypothesis on the relationship between exogenous and endoge-nous variables (γ) or among endogenous variables (β). In summary, perceived stress, family adapta-bility, and cohesion, social support, resilience, and social function directly affect CHR, and coping has an indirect influence via resilience, with 14 hypo-thetical pathways in total (Figs. 1, 2).
Introduction
- 1. Study design
- This study adopted a structural model approach that constructs a hypothetical model based on ARM, SVM, and a preceding study to check the influence on CHR and verify the fit of the model.
- 2. Study population
- Subjects were healthy individuals aged 18∼35, which is early adulthood, who are literate and capable of completing the online survey. Sample size was calculated using G-power 3.0, yielding 89 subjects. According to previous studies, assuming the possibility of including CHR at around 10% [18,19], a minimum of 890 subjects are necessary to procure sufficient power. In addition, since this study employed a questionnaire survey, 1,068 subjects (1.2×890) were selected as final subjects in consideration of the low recovery rate and dropout rate. A total of 1,068 subjects participa-ted, and those who had dismal response and clini-cal symptoms of schizophrenia or bipolar disorder were excluded, leaving 907 subjects to be included in the final analysis.
- 3. Study variables
- The Perceived Stress Scale (PSS) developed by Cohen et al. was used to measure perceived stress [23]. A total of 10 questions were rated on a 5-point Likert scale, with higher scores indicating higher perce-ived stress. Cronbach’s α was .84 in Chiu et al. [24] and .75 in the current study.
- The Family Adaptability and Cohesion Evaluation Scales-III (FACES-III) developed by Smith et al. was adopted to measure family adaptability and cohesion [25]. This included 20 questions on a 5-point Likert scale, with higher scores indicating higher perceived stress. Cronbach’s α was .83 at the time of development and .93 in the current study. Subcategories were family adaptability and family cohesion, with Cronbach’s α of .89 and .86, respectively.
- The Social Support Index (SSI) developed by McCubbin was used to measure social support [26]. This included 17 questions on a 5-point Likert scale, with higher scores indicating higher social support. Cronbach’s α was .82 at the time of development and .79 in the current study.
- The Brief Coping Orientation to Problems Experi-enced (Brief COPE) developed by Carver et al. was used to evaluate coping [27]. This included 28 questions on a 4-point Likert scale, with higher scores indicating higher coping. Cronbach’s α was .90 at the time of development and .81 in the current study. A total of 14 subcategories of coping strategies were grouped into three categories: defen-sive coping, positive coping, and derived meaning. Defensive coping included self-distraction, venting, behavioral disengagement, denial, substance use, and self-blame. Positive coping included positive reframing, active coping, use of emotional support, use of instrumental support, planning, acceptance, and humor. Derived meaning included religion. Cronbach’s α for defensive coping, positive coping, and derived meaning was .62, .65, and .33, respec-tively. The credibility of the derived meaning was too low; thus, religion was excluded, and the scores of only 13 subcategories of defensive coping and positive coping were included.
- The Brief Resilience Scale (BRS) developed by Smith et al. was implemented to evaluate resilience [28] This included six questions on a 5-point Likert scale, with higher scores indicating higher resilience. Cronbach’s α was .93 in Amat et al. [29] and .84 in the current study.
- The Global Assessment of Functioning (GAF) de-veloped by Söderberg et al. was utilized to eva-luate social function [30]. The GAF is a tool to evaluate the overall psychological and social function of the past one month. Scores range from 0 to 100, with higher scores indicating better overall function. GAF is commonly used in clinic due to its simplicity of single questions, and intraclass correlation coefficients (ICC) were .81 at the time of development.
- The Prodromal Questionnaire-Brief (PQ-B) deve-loped by Loewy et al. [22], which comprises 21 questions that record total and distress scores, was used to evaluate CHR. The distress score is measured only when the response to each que-stion is “Yes.” The higher the score on a 5-point Likert scale, the more likely CHR is. In Jang et al. and Xu et al., Cronbach’s α was .83 and .89, respectively [21,31], and .88 in the current study.
- 4. Data collection and ethical considerations
- Data were collected from February to March 2019, and a survey was conducted via SNS such as Facebook (www.facebook.com). A recruitment notice was posted on the website along with an address for the online-based survey for individuals who volunteered to participate. Subjects were selected using convenience sampling, and those who com-pleted the survey were given a small reward. This study was conducted after obtaining approval from the Institutional Review Board (IRB) of Korea University for credibility and validity of the research process and the rights of the subjects (KUIRB-2019-0045-01). In addition, for privacy and confidentiality of the subjects, identifiers such as name and phone number were anonymized.
- 5. Data analysis
- Analysis of all data was performed in SAS (statistical analysis system) 9.4 and AMOS 20.0, for Windows, and the maximum likelihood method was used. General characteristics of the subjects and descriptive statistics were shown in actual number, percentage, average, and standard deviation. AMOS 20.0 was used for model fit of the measurement model and multiple mediator effect to assess the calculated model fit index. The normed chi-square value, normed fit index (NFI), comparative fit index (CFI), Tucker-Lewis coefficient (TLI), goodness of fit index (GFI), and root mean square error of appro-ximation (RMSEA) were used as model fit indexes. In addition, the significance was verified by ana-lyzing the direct, indirect, and total effects of the exogenous variables of the modified model on the endogenous variables using the bootstrapping technique.
Materials and Methods
1) Perceived stress
2) Family adaptability and cohesion
3) Social support
4) Coping
5) Resilience
6) Social function
7) Clinical high risk
- 1. Demographic characteristics of the study population
- The subjects were healthy males and females aged 18∼35 years in early adulthood, and their general characteristics are reported in Table 1. Among the 907 subjects, 102 (11.25%) were classified as CHR. The normal group and CHR did not show statistically significant differences in terms of gender, age, region, religion, marriage, and household members.
- 2. Fit verification of hypothetical and revised models
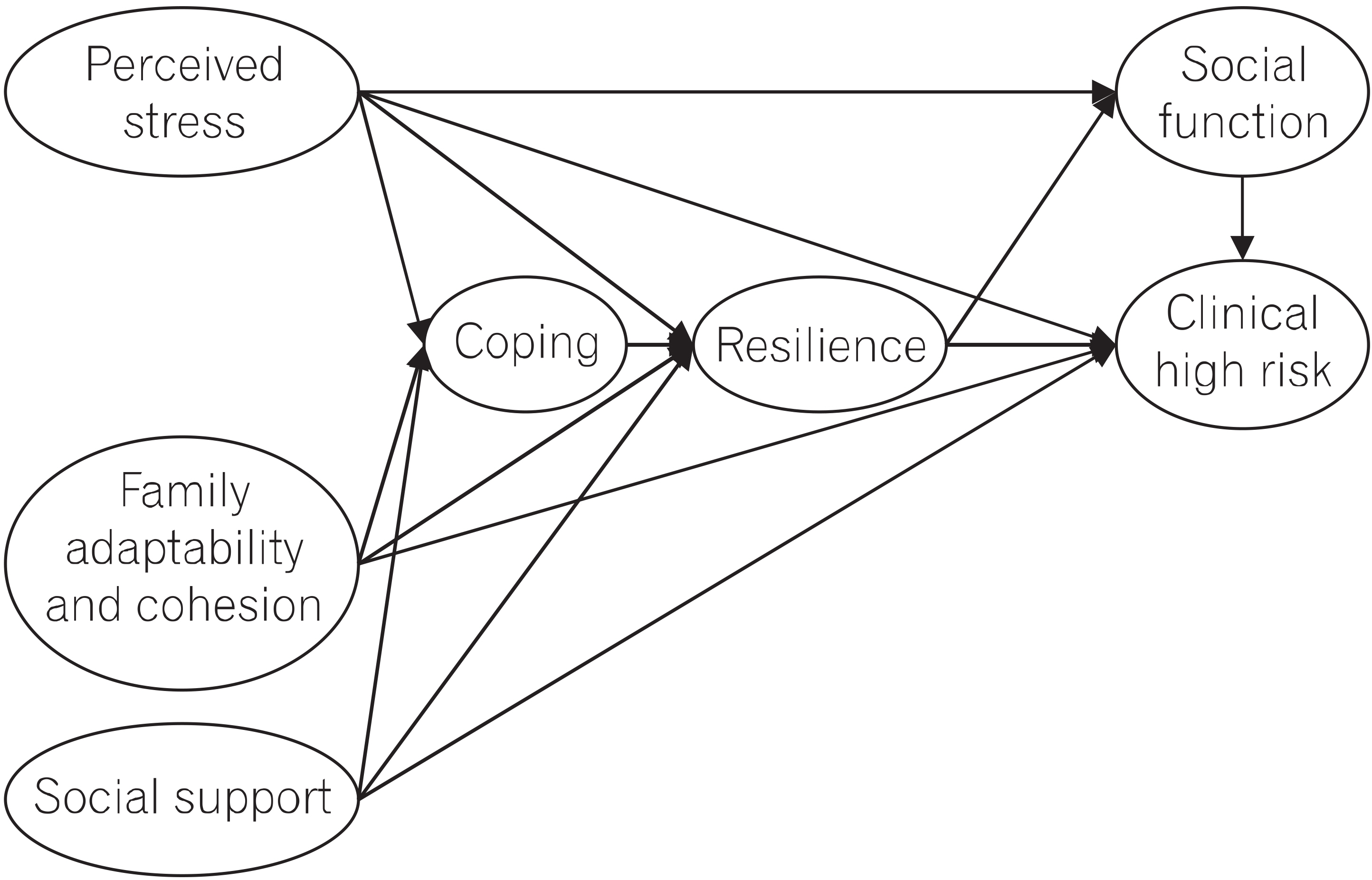
- The standard for the optimal model was .90 or higher GFI, AGFI, CFI, TLI, and IFI, with .08 or lower in model fit evaluation, and when RMSEA was .08 or lower, the model was considered excellent [32]. The chi-square (c2) value in the hypothetical model of CHR was 5.25, and GFI and AGFI were appropriate with .97 and .93, respectively. CFI, TLI, and IFI did not meet the standard, forcing us to revise the model (Table 2). The pathway from social support to resilience (t=1.33, p=.185), from social support to CHR (t=1.41, p=.159), and from family adaptation and cohesion (t=14, p=.892) were insignificant and therefore deleted. The pathway from coping to CHR (t=4.14, p<.001) showed a significant effect and was added, and derived meaning, a subcategory of coping, had low explanatory power and was deleted. Regarding the fit of the revised model, the chi-square (c2) value was 4.45, with GFI=.98, AGFI=.95, CFI=.92, TLI=.83, and IFI=.92, which mostly satisfied the standard value of .90 or more. RMSEA was .06, which was lower than the standard of the optimal model, .08, increasing the fitness of the model compared to the hypothetical model.
- 3. Estimation of pathway of revised model
- After analyzing the revised model, 12 pathways were found to be statistically significant (Fig. 3). Perceived stress (γ=.18, p<.001), family adaptation and cohesion (γ=.18, p=.001), and social support (γ=.41, p<.001) had a significant influence on coping. Perceived stress (γ=−.48, p<.001), family adap-tation and cohesion (γ=.18, p<.001), and coping (β=−.13, p=.002) had a significant influence on resilience. Perceived stress (γ=−.25, p=.001) and resilience (β=.16, p<.001) showed a significant influence on social function, while perceived stress (γ=.22, p<.001), coping (β=.14, p<.001), resilience (β=−.14, p<.001), and social function (β=−.22, p=.001) had a significant influence on CHR.
- 4. Mediated effect analysis on revised model
- Specific analysis results regarding direct, indirect, and total effects of the revised model are reported in Table 3.
- Perceived stress (γ=.18, p<.001), family adaptation and cohesion (γ=.18, p=.001), and social support (γ=.41, p<.001) had significant positive direct effects on coping, and the explanatory power of the variables was 29.0%. Perceived stress (γ=−.48, p<.001) and coping (β=−.13. p=.002) had a negative direct effect on resilience, whereas family adaptation and cohesion (γ=.18, p<.001) had a positive direct effect. Perceived stress (γ=−.02, p=.001) and family adaptation and cohesion mediated by coping (γ=−.02, p=.001) had negative indirect effects, and the explanatory power of these variables on resilience was 33.0%. Perceived stress (γ=−.25, p=.001) had a negative direct effect on social function, whereas resilience (β=.16, p<.001) had a positive direct effect. Perceived stress me-diated by coping and resilience (γ=−.08, p<.001) had a negative indirect effect. The explanatory power of the variables on social function was 13.0%. Perceived stress (γ=.22, p<.001) and coping (β= .14, p<.001) had positive direct effects on CHR, whereas resilience (β=−.14, p<.001) and social function (β=−.22, p=.001) had a negative direct effect. Perceived stress (γ=.17, p<.001) mediated by coping, resilience, and social function and co-ping mediated by social function (β=.02, p=.001) had a positive indirect effect, and resilience me-diated by social function (β=−.03, p=.001) showed a negative indirect effect. The explanatory power of the variables was 23.0%.
Results
- This study was conducted on healthy adult sub-jects to determine the factors influencing CHR using a structural model. Previous studies on CHR have mostly been based on retrospective evaluation of outpatients or inpatients, and only a few studies have focused on healthy general popu-lations. Despite some difficulty in directly com-paring the outcome of the study, discussion is mainly focused on the core content. In the revised model, the explanatory power of per-ceived stress, coping, resilience, and social func-tion on CHR was 23.0%. Confirming the signi-ficant pathway between each factor and CHR, variables such as perceived stress, coping, resi-lience, and social function were found to have a direct influence, while those such as family adap-tability and cohesion and social support had in-direct effects.
- When examined structurally, perceived stress has a direct and positive effect on CHR, and the higher the perceived stress, the higher the risk of CHR. This is consistent with the results of a number of previous studies [8,10,33], suggesting that perceived stress is the initiator as well as a catalyst in CHR [6,9]. Therefore, as perceived stress can be a meaningful indicator to prevent the occurrence of CHR in early adulthood, it is necessary to develop a program of education and intervention skills to relieve and manage stress.
- Second, coping was found to have a direct positive effect on the CHR group, which can be inter-preted to mean that the more the coping beha-vior is taken, the higher the CHR. Coping had a positive effect on perceived stress. This can be interpreted as an effort to control the threat and reduce or overcome stress by implementing coping actions as an adaptation strategy to protect the ego when facing harmful stress [34]. Chisholm et al. reported that the higher the stress, the more avoidant coping strategies were used as a response [35]. Kang et al. reported that schizophrenic pa-tients used more active coping [36]. Das et al. suggested that patients with schizophrenia emplo-yed a positive reframing strategy more often [37]. However, Moritz et al. reported that schizoph-renic patients lacked coping compared to the con-trol group, which is contrary to the results of the current study [38]. Ham and Sung reported that the degree of coping with stress differed based on the severity of the symptoms experienced by the subject [39]. In other words, there was no difference in coping methods in the early stages of schizo-phrenia; however, in the mid-term, passive coping was commonly used, and active coping was used in the next stage. Hasse also suggested that when coping with perceived stress, defensive coping is temporarily used in the initial stage, but positive coping is continuously used afterwards [22]. However, since the subjects of this study were not mentally ill, it is difficult to estimate which coping tech-nique is particularly effective as the severity of symptoms is not presented, unlike previous studies. Therefore, in future studies, it will be necessary to evaluate the severity of symptoms when deter-mining the degree of coping with CHR.
- Third, resilience has a direct negative effect on CHR, which can be interpreted as the lower the resilience, the higher the risk of CHR. In the structural model, it was found that when the perceived stress increased, the subjects' coping strategies became active. However, as this has a positive relationship with CHR, it acts as a pro-tective factor against perceived stress, but it is presumed that these coping behaviors alone do not control stress. Rather, resilience showed a negative relationship with perceived stress and a negative relationship with CHR, which suggested that resilience acted as a buffer element against stress [40]. Resilience is innate and refers to the positive power to overcome stress or adversity inherent in an individual [8,9,41]. Therefore, it is difficult to directly strengthen resilience, but it is necessary to find strategies to promote its growth by identifying factors that influence it, such as experiences of various stimuli, deep reflection, family support, and interpersonal relationships, from various angles.
- Fourth, social function has a direct negative effect on CHR, and lower social function is asso-ciated with a higher risk of becoming CHR. Social function has an advantage in that unlike other variables, it can be easily confirmed [42]. In other words, perceived stress, family adaptability and co-hesion, social support, coping, and resilience are imperceptible factors, making it difficult to notice unless they are evaluated using an objective tool. However, as social dysfunction is apparent, it is highly regarded as a predictor for early detection of CHR because it can be noticed to some extent by non-professionals [8]. In the structural model, the risk was high in people with low social function. Subjects with higher perceived stress showed lower social function, whereas higher resilience was accompanied by higher social function. Therefore, it can be concluded that the evaluation of social function is critical in the prevention of CHR.
- A structural model was established and tested for multidimensional clarification of the factors influencing the CHR with the goal of detecting and preventing schizophrenia at an early stage. However, there is a limitation in not being able to measure genetic factors or biological indicators, which are the most important factors in the develo-pment of schizophrenia. These key indicators were not included as this study aimed at early detection of schizophrenia in healthy adults within the com-munity, making it impossible to suggest genetic or biological marker testing for each subject. In addition, since this study required a large number of samples nationwide as a descriptive research study, an internet-based questionnaire was employed, which has the advantage of obtaining a large number of samples in a short period of time and completing the survey in a short time as a relatively simple response is required. However, there have been cases where responses are incomplete, and even if they are complete, 161 cases (15.1%) were not included in the statistics because their responses were deemed not sincere. The selected subjects participated after reading the purpose of the study only as a simple explanatory text, making it insufficient to guarantee the complete validity of the responses. Therefore, to increase both the response rate and validity, future research should consider more specialized face-to-face surveys. This study employed measurement tools mainly implemented for schizophrenia in previous research but may not have sufficient explanatory power because the subjects were selected from the general public.
- As full remission of schizophrenia is difficult and the condition tends to become chronic, early detection and minimizing the untreated period is crucial. However, regarding preventive means, a more aggressive approach to screen CHR among the general population is necessary as studies on patients already suffering from schizophrenia have limitations. Thus, this study identified factors that affect CHR in early adulthood and explained the mechanism using a structural model. Based on the results, the variables that directly affect coping in the modified model are perceived stress, family adaptation and cohesion, and social support, and those that directly affect resilience are perceived stress, family adaptation and cohesion, and coping. The variables directly influencing social function are perceived stress and resilience, whereas perceived stress, family cohesion, coping, resilience, and so-cial function have significant direct effects on CHR. Based on the results, the following suggestions are proposed.
- First, although the current study is based on sub-jects in early adulthood, subsequent studies should target those in adolescence for more aggressive early intervention.
- Second, the selected tool of investigation may have a limitation of insufficient explanatory power for general populations; it is therefore suggested that future studies use more appropriate tools.
Discussion
Acknowledgments
Acknowledgements
Table 1General characteristics of participants N=907
Table 2Comparison of model fit of modified model to hypothetical model
| Model | χ2 (p) | df | Normed χ2 | GFI | AGFI | CFI | TLI | IFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|
| Hypothetical model | 120.72 (<.001) | 23 | 5.25 | .97 | .93 | .87 | .75 | .88 | .07 |
| Modified model | 75.64 (<.001) | 17 | 4.45 | .98 | .95 | .92 | .83 | .92 | .06 |
Table 3Standardized direct, indirect, and total effects of the modified model
- 1. Jeong YR, Yoo TY, Lee JY, Kim SY, Yoon JS, Kim SW. 2017;Factors related to Internalized stigma in patients with schizophrenia. Journal of the Korean Society of Biological Therapies in Psychiatry. 23(2):37-45. http://doi.org/10.22802/jksbtp.2017.23.2.75Article
- 2. Aikawa S, Kobayashi H, Nemoto T, Matsuo S, Wada Y, Mamiya N, et al. 2018;Social anxiety and risk factors in patients with schizophrenia: Relationship with duration of untreated psychosis. Psychiatry Research. 263:94-100. https://doi.org/10.1016/j.psychres.2018.02.038.ArticlePubMed
- 3. Jeon IH, Park JS, Park JY, Cho HH, Koo SJ, Lee E, et al. 2012;Working memory deficits in ultra-high risk for psychosis and schizophrenia. Korean Journal of Schizophrenia Research. 15(2):66-72. https://doi.org/10.16946/kjsr.2012.15.2.66Article
- 4. An SK. 2018;Ultra-high risk for psychosis: Clinical characteristics and diagnosis. Journal of Korean Neuropsychiatric Association. 57(3):210-224. https://doi.org/10.4306/jknpa.2018.57.3.210Article
- 5. Oliver EA, Fearon P. 2008;Schizophrenia: Epidemiology and risk factors. Psychiatry. 7(10):410-414. https://doi.org/10.1016/j.mppsy.2008.07.011Article
- 6. Fusar-Poli PM, Tantardini M, De Simone S, Ramella-Cravaro V, Oliver D, Kingdon J, et al. 2017;Deconstructing vulnerability for psychosis: Meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. European Psychiatry. 40:65-75. https://doi.org/10.1016/j.eurpsy.2016.09.003.ArticlePubMed
- 7. Sung KM. 2017;A theoretical structural model for caring persons with early psychosis: A systematic review and qualitative meta analysis. Journal of the Korea Academia-Industrial Cooperation Society. 18(1):66-74. https://doi.org/10.5762/KAIS.2017.18.1.66Article
- 8. Georgiades A, Farquharson L, Ellett L. 2015;Resilience recovery style, and stress in early psychosis. Psychosis. 7(2):183-185. https://doi.org/10.1080/17522439.2014.936028Article
- 9. Zubin J, Spring B. 1977;Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology. 86(2):103-126. https://doi.org/10.1037/0021-843X.86.2.103.ArticlePubMed
- 10. Renwick L, Jackson D, Turner N, Sutton M, Foley S, McWilliams S, et al. 2009;Are symptoms associated with increased levels of perceived stress in first-episode psychosis? International Journal of Mental Health Nursing. 18(3):186-194. https://doi.org/10.1111/j.1447-0349.2009.00600.x.ArticlePubMed
- 11. Secades XG, Molinero O, Salguero A, Barquín RR, de la Vega RL, Márquez S. 2016;Rela-tionship between resilience and coping strategies in competitive sport. Perceptual and Motor Skills. 122(1):336-349. https://doi.org/10.1177/0031512516631056.ArticlePubMed
- 12. Mäki P, Koskela S, Murray GK, Nordström T, Miettunen J, Jääskeläinen E. 2014;Difficulty in making contact with others and social withdrawal as early signs of psychosis in adolescents-the Northern Finland Birth Cohort 1986. European Psychiatry. 29(6):345-351. https://doi.org/10.1016/j.eurpsy.2013.11.003.ArticlePubMed
- 13. Skuhareuskaya M, Skugarevsky O. 2017;Predictors of transition to psychosis in individuals at clinical high-risk for psychosis. European Psychiatry. 41(S1):s838-s838. https://doi.org/10.1016/j.eurpsy.2017.01.1651Article
- 14. Fond G, Boyer L, Andrianarisoa M, Godin O, Brunel L, Bulzacka E, et al. 2018;Risk factors for increased duration of untreated psychosis. Results from the FACE-SZ dataset. Schizophrenia Research. 195:529-533. https://doi.org/10.1016/j.schres.2017.08.058.ArticlePubMed
- 15. Gurak K, Weisman de Mamani AW. 2016;Risk and protective factors perceptions of family environment ethnicity and schizophrenia symptoms. Journal of Nervous and Mental Disease. 204(8):570-577. https://doi.org/10.1097/NMD.0000000000000558.ArticlePubMed
- 16. Santayana GPd, Landera R, Juncal M, Porta O, Gómez M, Núñez N, et al. 2017;Ultra-high risk psychosis: A case report. European Psychiatry. 41(S1):S730-S731. https://doi.org/10.1016/j.eurpsy.2017.01.1335Article
- 17. Larsen TK, Melle I, Auestad B, Haahr U, Joa I, Johannessen JO. 2011;Early detection in psychosis: 5 year outcome in the Scandinavian tips-study. European Psychiatry. 26(1):2010https://doi.org/10.1016/S0924-9338(11)73713-0Article
- 18. Kim SW, Chung YC, Kang YS, Kim JK, Jang JE, Jhon M, et al. 2018;Validation of the Korean version of the 16-item prodromal questionnaire in a non-help-seeking college population. Psychiatry Investigation. 15(2):111-117. https://doi.org/10.30773/pi.2017.04.24.ArticlePubMed
- 19. Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD. 2011;Psychosis risk screening with the prodromal questionnaire -brief version (PQ-B). Schizophrenia Research. 129(1):42-46. https://doi.org/10.1016/j.schres.2011.03.029.ArticlePubMed
- 20. Opier MGA, Perrin M, Kleinhaus K, Malaspina D. 2008;Factors in the etiology of schizophrenia: Genes, parental age, and environment. Primary Psychiatry,. 15(6):37-45.
- 21. Xu LH, Zhang TH, Zheng LN, Li HJ, Tang YY, Luo XG, et al. 2016;Psychometric properties of prodromal questionnaire-brief version among Chinese help-seeking individuals. PLOS ONE. 11(2):e0148935. https://doi.org/10.1371/journal.pone.0148935.ArticlePubMedPMC
- 22. Haase JE. 2004;The adolescent resilience model as a guide to interventions. Journal of Pediatric Oncology Nursing. 21(5):289https://doi.org/10.1177/1043454204267922.ArticlePubMed
- 23. Cohen S, Kamarck T, Mermelstein R. 1983;A global measure of perceived stress. Journal of Health and Social Behavior. 24(4):385https://doi.org/10.2307/2136404.ArticlePubMed
- 24. Chiu YH, Lu FJH, Lin JH, Nien CL, Hsu YW, Liu HY. 2016;Psychometric Properties of the Perceived Stress Scale (PSS): Measurement invariance between athletes and non-athletes and construct validity. Peer Journal. 4(e2790):14-34. https://doi.org/10.7717/peerj.2790.Article
- 25. Smith SG. 1996, Clinical utility of the Family Adaptation and Cohesion Evaluation Scales III (FACES III). Texas Tech University; Texas.
- 26. McCubbin HI, Patterson J, Glynn T. In J Fischer, Corcoran, J Kevin (Eds.),1982, Social Support Index (SSI). Measures for clinical practice and research: A sourcebook. 4th edition. Oxford University; New York, NY: p. 413-414.
- 27. Carver CS. 1997;You want to measure coping but your protocol’s too long consider the brief COPE. International Journal of Behavioral Medicine. 4(1):92-100. https://doi.org/10.1207/s15327558ijbm0401_6ArticlePubMed
- 28. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. 2008;The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine. 15(3):194-200. https://doi.org/10.1080/10705500802222972.ArticlePubMed
- 29. Amat S, Subhan M, Marzuki Wan Jaafar W, Mahmud Z, Suhaila Ku Johari K. 2014;Evaluation and psychometric status of the brief resilience scale in a sample of Malaysian international students. Asian Social Science. 10(18):240-245. https://doi.org/10.5539/ass.v10n18p240Article
- 30. Söderberg P, Tungström S, Armelius BA. 2005;Reliability of global assessment of functioning ratings made by clinical psychiatric staff. Psychiatric Services. 56(4):434-438. https://doi.org/10.1176/appi.ps.56.4.434.ArticlePubMed
- 31. Jang YE, Lee TY, Hur JW, Kwon JS. 2019;Validation of the Korean version of the prodromal questionnaire-brief version in non-help-seeking Individuals. Psychiatry Investigation. 16(2):109-114. https://doi.org/10.30773/pi.2018.10.23.ArticlePubMedPMC
- 32. Kang HC. 2013;Discussions on the suitable interpretation of model fit indices and the strategies to fit model in structural equation modeling. Journal of the Korean Data Analysis Society. 15(2):653-668.
- 33. Arya R. 2017;Understanding the coping behaviour of person suffering from sexual deviation and dysfunctions. International Journal of Indian Psychology. 4(3):123-132. https://doi.org/10.25215/0403Article
- 34. Ruzibiza C, Grattan RE, Rebekah ER, Linscott RJ. 2018;Components of schizophrenia liability are not uniformly associated with stress sensitivity resilience and coping. Psychiatry Research. 260:10https://doi.org/10.1016/j.psychres.2017.11.039ArticlePubMed
- 35. Chisholm KE, Wigman JTW, Hallett D, Woodall T, Mahfouda S, Reniers RLEP, et al. 2018;The role of coping in the association between subclinical psychotic experiences and functioning: A within study replication in two independent adolescent samples. Schizophrenia Research. 201:91-97. https://doi.org/10.1016/j.schres.2018.05.022.ArticlePubMed
- 36. Kang MJ, Bang MJ, Lee SY, Lee E, Yoo SW, An SK. 2018;Coping styles in individuals at ultra- high risk for psychosis: Associations with cognitive appraisals. Psychiatry Research. 264:162-168. https://doi.org/10.1016/j.psychres.2018.03.079.ArticlePubMed
- 37. Das S, Punnoose VP, Doval N, Nair VY. 2018;Spirituality religiousness and coping in patients with schizophrenia: A cross sectional study in a tertiary care hospital. Psychiatry Research. 265:238-243. https://doi.org/10.1016/j.psychres.2018.04.030.ArticlePubMed
- 38. Moritz S, Lüdtke T, Westermann S, Hermeneit J, Watroba J, Lincoln TM. 2016;Dysfunctional coping with stress in psychosis. An investigation with the maladaptive and adaptive coping styles (MAX) questionnaire. Schizophrenia Research. 175(1-3):129-135. https://doi.org/10.1016/j.schres.2016.04.025.ArticlePubMed
- 39. Ham JH, Sung KM. 2016;A study on stress coping skill suicide risk and suicidal ideation according to treatment phases of hospitalized patients with schizophrenia. Journal of Korean Academy of Psychiatric and Mental Health Nursing. 25(4):338-346. https://doi.org/10.12934/jkpmhn.2016.25.4.338Article
- 40. Drvaric L, Gerritsen C, Rashid T, Bagby RM, Mizrahi R. 2015;High stress, low resilience in people at clinical high risk for psychosis: Should we consider a strengths-based approach? Canadian Psychology/Psychologie Canadienne. 56(3):332-347. https://doi.org/ 10.1037/cap0000035Article
- 41. Torgalsbøen AK, Fu S, Czajkowski N. 2018;Resilience trajectories to full recovery in first-episode schizophrenia. European Psychiatry. 52:54-60. https://doi.org/10.1016/j.eurpsy.2018.04.007.ArticlePubMed
- 42. Barrios M, Gómez-Benito J, Pino O, Rojo E, Guilera G. 2018;Functioning in patients with schizophrenia: A multicentre study evaluating the clinical perspective. Psychiatry Research. 270:1092-1098. https://doi.org/10.1016/j.psychres.2018.05.079.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 



 PubReader
PubReader Cite
Cite