Articles
- Page Path
- HOME > STRESS > Volume 28(1); 2020 > Article
-
Review Article
제 2형 당뇨병 노인의 우울증상과 혈당조절에 대한 지역사회 기반 심리 중재의 효과: 체계적 문헌고찰과 메타분석 -
유혜진
 , 황보영
, 황보영
- Effects of Community-Based Psychological Interventions on Depressive Symptoms and Blood Glucose Control for Older Individuals with Type 2 Diabetes: A Systematic Review and Meta-Analysis
-
Heajin Yu
 , Boyoung Hwang
, Boyoung Hwang
-
stress 2020;28(1):1-9.
DOI: https://doi.org/10.17547/kjsr.2020.28.1.1
Published online: March 31, 2020
1 서울대학교 간호대학, 시립은평병원
2 서울대학교 간호대학, 간호과학연구소
1College of Nursing, Seoul National University & Seoul Metropolitan Eunpyeong Hospital, Seoul, Korea
2College of Nursing & The Research Institute of Nursing Science, Seoul National University, Seoul, Korea
- Corresponding author Heajin Yu, College of Nursing, Seoul National University, 103 Daehak-ro, Jongro-gu, Seoul 13080, Korea, Tel: +82-2-740-8477, Fax: +82-2-740-8477, E-mail: heajinyu@snu.ac.kr
• Received: July 15, 2019 • Revised: February 13, 2020 • Accepted: February 14, 2020
Copyright © 2020 by stress. All rights reserved.
- 2,343 Views
- 117 Download
- 1 Crossref
Key messages
-
Background
- To review the effects of community-based psychological interventions on depressive symptoms and blood glucose levels of older individuals with type 2 diabetes (T2D).
-
Methods
- A literature search was conducted using seven electronic databases (CINAHL, EMbase, PubMed, CENTRAL, KoreaMed, KISS, and KMbase). The main search terms were ‘diabetes’, ‘depression’, ‘older adult’, and ‘psychological intervention’. The search was restricted to peer-reviewed RCTs published between January 1, 2008 and July 31, 2018.
-
Results
- Five studies with a total of 596 participants met the inclusion criteria. Four studies that were included in the meta-analysis incorporated some form of behavioral strategies. Depressive symptoms were measured in four of the five studies, and HbA1c was measured in two of the five studies. The pooled SMD for depressive symptoms was −0.13 (95% CI, −0.31, 0.04; p=0.13) and −0.63 (95% CI, −0.98, −0.28; p<0.001) for HbA1c.
-
Conclusions
- This review highlights the need for additional clinical trials for psychological interventions in older individuals with T2D, especially trials on a larger scale with a wider geographical scope.
Abstract
- 본 연구에서는 노인 당뇨 환자를 대상으로 한 지역사회 기반 심리 중재가 환자들의 우울 증상과 혈당조절에 미치는 효과를 체계적으로 고찰하였다. 국내외 7개의 데이터베이스를 사용하여, 2008년 1월 1일부터 2018년 7월 31일까지 발표된 문헌들을 확인하였다. 선정기준에 따라 다섯 편의 연구가 최종 선정되었으며, 총 대상자는 제2형 당뇨 진단을 받은 지역사회 거주 노인 596명이었다. 메타분석에 선정된 네 편의 연구 모두 행동 교육을 목적으로 프로그램을 구성하였다. 추후에는 표본 크기를 늘려 심리적 중재 프로그램을 시행하는 것이 바람직하며 더욱 다양한 지역에서 수행하는 것이 필요함을 확인할 수 있었다.
- Diabetes mellitus (DM) is a serious health condition that is approaching epidemic proportions (Hu, 2011). According to the World Health Organization (WHO), roughly 400 million adults are diagnosed with DM worldwide (World Health Organization [WHO], 2016). T2D results from the abnormal regulation of glucose metabolism and is known to be the most common type of DM. The risk of T2D increases with advancing age, and therefore, it is approximately eight times more prevalent in the older population than in younger adults.
- With its increasing prevalence and the aging of the population, it is estimated that the number of older individuals diagnosed with T2D will increase more than fourfold from 2005 to 2050 (Kirkman et al., 2012). This indicates that T2D will continue to be a considerable burden on healthcare systems and societies (de Vries et al., 2016).
- T2D is a chronic, debilitating disorder that affects various body systems simultaneously, resulting in serious complications. Some of the major complications of T2D are neuropathy, nephropathy, retinopathy, and macrovascular problems (Sjostrom et al., 2014). In addition to these physiological complications, depression is a common comorbidity.
- Approximately 18% of diabetic patients have diabetes-specific emotional distress, and 20 to 40% of them end up being diagnosed with depression (Mushtaque et al., 2016). Depression in DM negatively affects the patient’s physical and mental functioning, which results in difficulty controlling hemoglobin A1c (HbA1c) and following recommendations for diet, exercise, and self-care (de Vries et al., 2016).
- Psychological well-being is one of the ultimate goals of holistic diabetes management, yet little attention has been given to the psychological implications of DM. Psychological interventions are a subset of non-pharmacological interventions in diabetes management and have been shown to be effective in decreasing symptoms of depression and blood glucose levels (Safren et al., 2013; Chapman et al., 2015). There is increasing evidence of the acceptability and feasibility of community-based psychological interventions for individuals with DM, but evidence of their effectiveness is yet to be explored, especially for older individuals (Beverly et al., 2013).
- The vast majority of older individuals dwell in community settings. Most visit their primary health care providers for the management of DM. However, there is a major barrier in the form of very limited time availability for comprehensive care (Glasgow et al., 2004). Studies have shown that various interventions for older diabetic individuals are available in community settings. Community-based programs that focused on dietary changes, exercise, health behavior changes, and psychological support (including psychological interventions) have shown substantial benefits in the prevention and management of T2D (Shirinzadeh et al., 2019).
- However, no systematic review to date has been conducted to synthesize the effects of community-based psychological interventions for depressive symptoms and blood glucose levels in the older diabetic population. The purpose of this systematic review and meta-analysis was to review the effects of community-based psychological interventions among older diabetic adults on depressive symptoms and blood glucose levels. The specific aims were: 1) to identify the types of psychological interventions used for older diabetic individuals in community or outpatient settings; and 2) to determine the effectiveness of psychological interventions on depressive symptoms and blood glucose levels in older diabetic individuals.
Introduction
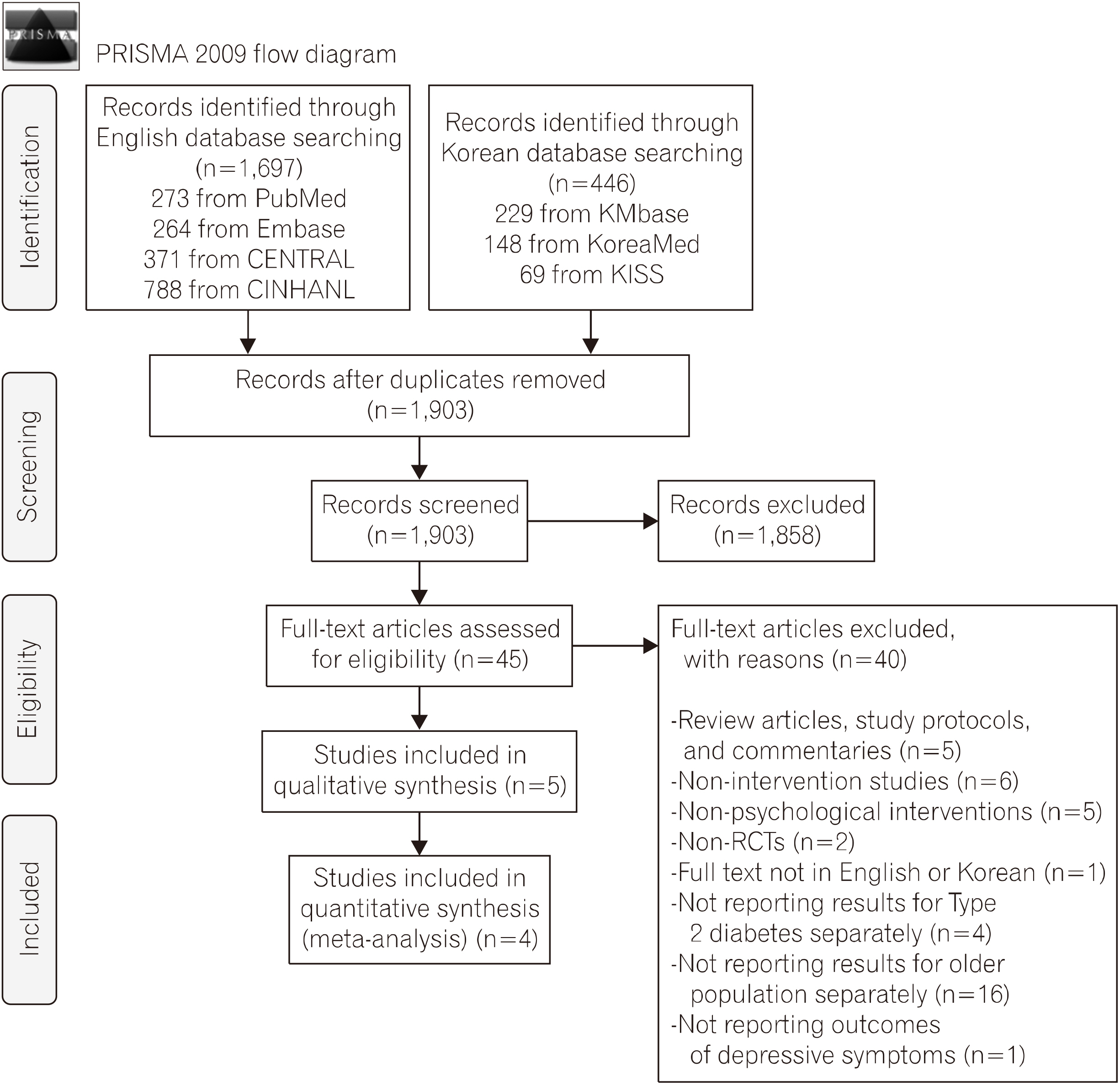
- This study was conducted following the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines for systematic reviews of interventions (Cochrane Handbook, 2018).
- 1. Eligibility criteria and study selection
- Studies were included in the review if the following criteria were met: 1) studies that focused on adults with T2D; 2) studies that included older adults (aged 60 years or older) only, or reported results from a subgroup of adults aged 60 years or older; 3) primary research studies that investigated psychological interventions; 4) studies that included the outcomes of depressive symptoms; 5) studies that tested the effects of psychological interventions in community settings; 6) RCTs; and 7) studies published in English or Korean. In this review, the term “psychological interventions” was defined as psychological therapies based on psycho-therapeutic principles, such as cognitive-behavioral therapy (CBT), non-directive counseling, motivational interviewing, and supportive therapy (Ismail et al., 2004).
- 2. Search strategy
- We systematically searched seven electronic databases to identify relevant and eligible research trials. Studies published in English were identified by searching Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), EMbase, PubMed, and KoreaMed. In the following databases, the search terms were entered in Korean: Korean Studies Information Service System (KISS) and Korean Medical Database (KMbase).
- The search queries within each electronic database were created based on the PubMed Clinical Queries. The search was restricted to peer-reviewed RCTs published between January 1, 2008 and July 31, 2018. Search terms included: “type 2 diabetes”, “diabetes mellitus”, “diabetes”, “adult onset diabetes mellitus”, “community-based psychological interventions”, “aged”, “older patients”, “elderly patients”, “depression”, “emotional depression”, “depressive symptoms”, “psychological intervention”, “psychotherapy”, “therapy”, and “program.” All of these search terms were then exploded to increase the search yield. Controlled vocabularies, such as Medical Subject Headings (MESH), EMTREE terms, and CINHAL subject headings, were used along with free-text terms. Only free-text terms were combined when searching in Korean databases.
- 3. Data collection and analysis methods
- Eligible studies were identified by both authors and inter-rater reliability was reported by using Cohen’s K (Mchugh, 2012). The degree of inter-rater reliability agreement between the reviewers was moderate (Cohen’s K=0.56; 95% CI, 0.19, 0.92). Disagreements were resolved by discussion. The data were extracted and coded in a standard way for the study sample and the characteristics of therapy in the intervention and control group. Pertinent data of the trial characteristics were extracted using the Cochrane’s review data extraction form. Effect sizes were calculated to assess the effectiveness of psychological interventions on depressive symptoms and glycemic controls using Review Manager 5.3 software (RevMan). The overall effect size was estimated by calculating the weighted mean difference, 95% confidence intervals, and standardized mean differences (SMD). For the computational model, the fixed-effect model was applied since the data were homogeneous (common true treatment effect).
- For the sake of completeness, Cochran’s Q-test and Higgins’ I2 statistics were used to quantify statistical heterogeneity. Before using these statistical methods, forest plots were used to see the directions of the effect sizes and confidence intervals and whether they were overlapping. Higgins’ I2 values of 25%, 50%, and 75% were set as representing low, moderate, and high heterogeneity, respectively (Higgins et al., 2001).
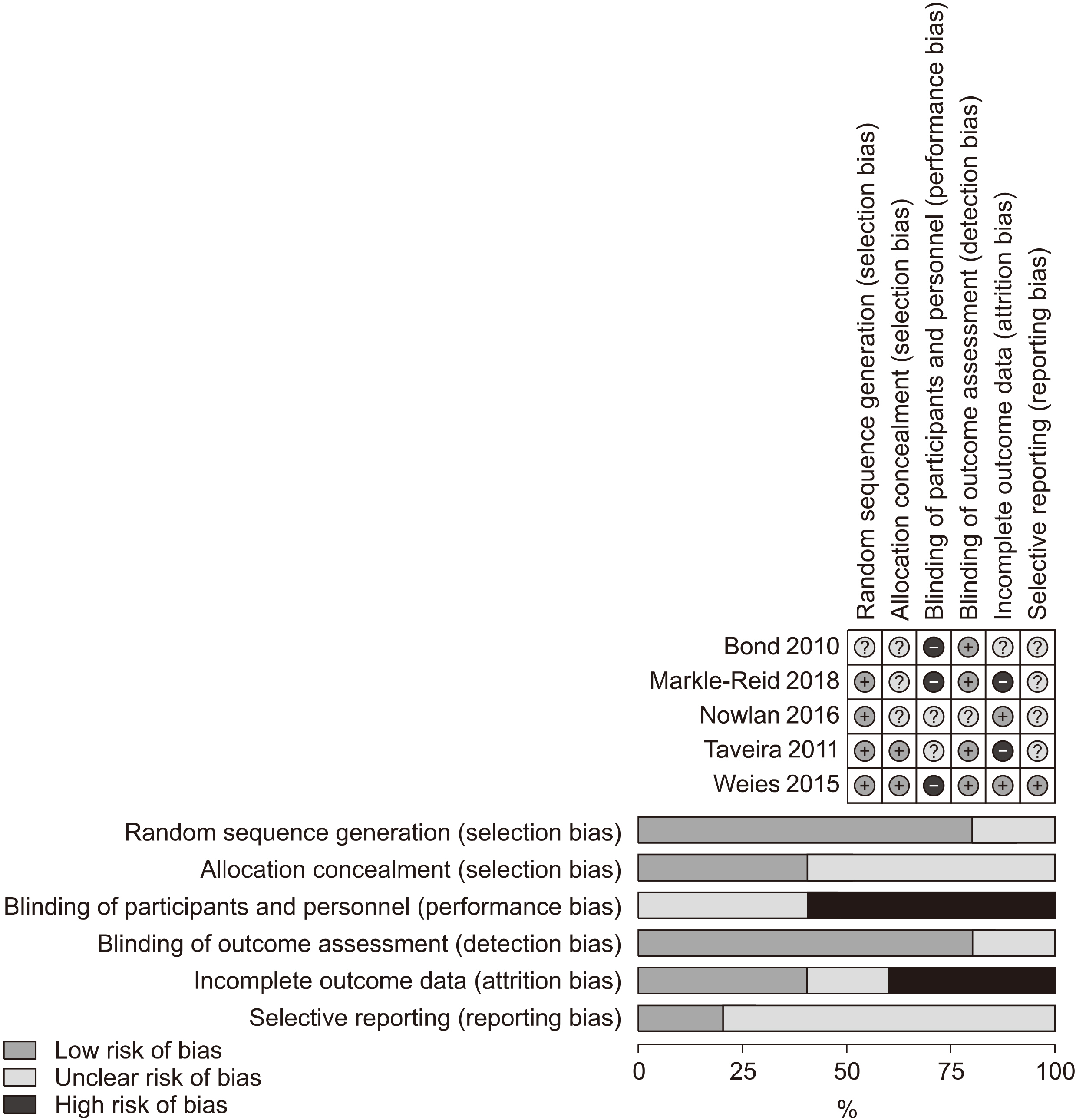
- 4. Risk of bias assessment
- To assess the quality of each study, we used the Cochrane RoB, which assesses five different areas: sequence generation, allocation concealment, blinding of outcome assessors, incomplete outcome data, and selective outcome reporting (Cochrane Handbook, 2018). Both authors independently rated bias using the selection process. Any discrepancies were resolved through discussion. The level of agreement (Mchugh, 2012) was excellent (intraclass correlation coefficient, 0.89, 95% CI, 0.78, 0.95).
Materials and Methods
- The initial search yielded 2,143 articles (Fig. 1). After all duplicates were eliminated, a total of 1,903 abstracts and titles were reviewed. A total of 45 RCTs were included for full-text review. Five RCTs (Bond et al., 2010; Taveira et al., 2011; Nowlan et al., 2015; Weiss et al., 2015; Markle-Reid et al., 2018) were included in a qualitative literature synthesis and a description of changes in depressive symptoms and blood glucose controls. Among those excluded from the review, there were five RCTs of intervention programs for community-residing older adults with T2D. These studies did not meet the inclusion criteria because the interventions were non-psychological in nature. Specifically, the following intervention programs were tested in these studies: peer advisor program (Baksi et al., 2008), pharmacotherapy (Bogner et al., 2010), diabetes education (Gagliardino et al., 2013), patient prioritized planning (de Vries et al., 2016), and nurse-administered pharmacological intervention (Lamers et al., 2011). Among the five RCTs included in the qualitative synthesis, one study (Nowlan et al., 2015) that did not report variance data was excluded from the quantitative literature synthesis.
- 1. Participant characteristic
- Table 1 summarizes the key characteristics of the studies that were included in the review. Five studies (Bond et al., 2010; Taveira et al., 2011; Nowlan et al., 2015; Weiss et al., 2015; Markle-Reid et al., 2018) with a total of 569 participants met the inclusion criteria. Sample sizes ranged from 62 to 206 (median, 88). The participants’ mean age ranged from 60.2 to 72.8 (median, 66.5) years. Approximately 40% of the participants were female. Four of the studies reported the length of time that participants had T2D, with the range being 7.4 to 20 years.
- 2. Study characteristics
- The publication years ranged between 2007 and 2018, and three (Nowlan et al., 2015; Weiss et al., 2015; Markle-Reid et al., 2018) of the five studies were published within the last five years. The studies were conducted in three countries: The United States (n=3), Canada (n=1), and Australia (n=2). The average length of the intervention period was 8.2 (1∼45) weeks, and the average number of intervention sessions was 7 (1∼13). In three (Bond et al., 2010; Nowlan et al., 2015; Weiss et al., 2015) out of the five studies, interventions were delivered individually. The remaining two (Bond et al., 2010; Taveira et al., 2011) were delivered in web-based and group formats, respectively. The psychological interventions tested in four studies (Bond et al., 2010; Taveira et al., 2011; Weiss et al., 2015; Markle-Reid et al., 2018) incorporated some form of behavioral strategies, and one study (Nowlan et al., 2015) included positive reappraisal. In three out of the five studies (Bond et al., 2010; Taviera et al., 2011; Markle-Reid et al., 2018), the control group received usual care or standard treatment. In the remaining two studies placebo therapy (Weiss et al., 2015) and an alternative intervention (Nowlan et al., 2016) were provided to the control group, respectively.
- The participants were recruited from diabetes centers or healthcare clinics in five RCTs (Bond et al., 2010; Taveira et al., 2011; Nowlan et al., 2015; Weiss et al., 2015; Markle-Reid et al., 2018). In all trials, outcomes were measured at baseline and at six-month follow-up. Four measures of depressive symptoms were identified: The Patient Health Questionnaire-9 (PHQ-9), Geriatric Depression Scale (GDS), Center for Epidemiologic Studies Depression Scale (CES-D), and 10-item Center for Epidemiologic Studies Depression Scale (CES-D-R). To measure blood glucose control, HbA1c levels were used in the studies.
- 3. Risk of bias
- Figure 2 presents details on the quality assessment of the included studies.
- Of the five RCTs, four (80%) adequately described their randomization sequence (Bond et al., 2010). Two of the five studies (40%) adequately demonstrated allocation concealment (Taveira et al., 2011; Weiss et al., 2015). Three studies (Bond et al., 2010; Nowlan et al., 2015; Markle-Reid et al., 2018) did not provide a clear description, so they were rated as unclear. Blinding of participants, personnel, and outcome assessors was not entirely possible for the included studies. In all five studies (Bond et al., 2010; Taveira et a l., 2011; Nowlan et al., 2015; Weiss et al., 2015; Markle-Reid et al., 2018), blinding of study personnel was not described; all were rated as either high or unclear. For the attrition bias assessment, only two studies (40%) were free from frequent missing data (Nowlan et al., 2015; Weiss et al., 2015). In the three remaining studies (Bond et al., 2010; Taveira et al., 2011; Markle-Reid et al., 2015, 2018), no information was provided concerning the attrition rate or reasons for missing data. Lastly, for the selective reporting assessment, one study (20%) provided a study protocol (Weiss et al., 2015). The other studies either provided insufficient information, or the study protocol could not be located.
- 4. Effectiveness of the interventions on depressive symptoms and blood glucose control
- Figure 3 shows the forest plots for the effect sizes of psychological interventions on depressive symptoms and blood glucose control, respectively. For depressive symptoms, there were four trials (515 participants) in the review with data that could be pooled. Individually, two studies showed statistically significant improvement in the intervention groups for depressive symptoms. In the fixed-effect model, the pooled SMD in the improvement of depressive symptoms between participants assigned to the psychological intervention group and those assigned to the control group was not statistically significant (d=0.13; 95% CI, −0.31, 0.04; p=0.31). The Cochrane Q and I2 scores indicated low heterogeneity (Q value=0.46; p=0.93; I2 =0%).
- HbA1c was measured in two of the five studies with 294 participants. Both studies reported improvement of HbA1c in the intervention group. At a six-month follow-up, HbA1c had fallen by 1.44% (from a baseline of 7.75%) in 147 participants in the intervention group and by 0.05% (from a baseline of 8%) among the remaining 147 participants in the control group. The pooled SMD of blood glucose control (HbA1c) was (d=0.63; 95% CI, −0.98, −0.28; p<0.001), indicating a medium effect size. The Cochran Q test and I2 scores for HbA1c (Q value=1.49, p=0.22, I2 =33%) indicated low to moderate heterogeneity.
- 5. Publication bias
- Tests of heterogeneity showed that the included studies were sufficiently homogeneous to be included in the meta-analysis. Due to the small number of studies, we were unable to assess publication bias.
Results
- We identified five RCTs that examined the effects of community-based psychological interventions on depressive symptoms and blood glucose levels in older individuals with T2D. The results were derived from studies involving 596 participants from three countries. The meta-analysis indicated that the effect size for depressive symptoms was small and not statistically significant. We found that psychological interventions had a significant overall effect in reducing blood glucose levels in older individuals with T2D. The effect was moderate in size. By means of a risk of bias assessment, most of the trials were rated as moderate in quality, and the overall statistical heterogeneity was low.
- To the best of our knowledge, this is the first systematic review of the effects of psychological interventions in community-dwelling older individuals with T2D. We used multiple types of electronic databases with a rigorous search strategy to identify eligible studies, which contributed to a higher sensitivity of the review. Moreover, the selection of eligible trials and quality assessment were completed independently by trained researchers, resulting in sufficient reliability. Even when only using a relatively small number of trials to perform the meta-analysis, it was possible to quantify the effect of depressive symptoms in conjunction with glycemic control. The low variance within the interventions and the lack of statistical heterogeneity of the findings indicate that the studies are highly consistent (Higgins, 2003).
- Our review has several limitations that need to be highlighted. First, all of the RCTs included were conducted in Western nations, whereas T2D is most prevalent in the South Pacific and Southeast Asia. Moreover, in two of the five studies, 97% of the participants were Caucasian, while all of the participants in another study were African-American. Therefore, the generalizability of our findings may be limited to populations with similar characteristics. Second, in all of the included studies, the method of blinding was not fully described or was unclear, which might have resulted in performance bias (Cochrane Handbook, 2018). Third, the methods of psychological intervention included in our meta-analysis were not uniform. However, because all four interventions had in common that their foundations were based on behavioral strategies and the overall heterogeneity of the studies was on the lower side, we proceeded to conduct a meta-analysis. Fourth, various types of comparison conditions were used in the studies and this may have affected study findings. Among the three studies that compared psychological interventions to usual care or standard treatment (Bond et al., 2010; Taviera et al., 2011; Markle-Reid et al., 2018), the intervention group had a significant reduction in depressive symptoms in two studies (Bond et al., 2010; Markle-Reid et al., 2018). No intervention effect on depressive symptoms was observed in the studies using placebo or alternative therapy as a comparison group (Weiss et al., 2015; Nowlan et al., 2016). Therefore, it is possible that the reduction in depressive symptoms may have resulted from non-specific therapeutic factors (i.e., the provision of attention, care, or social support) rather than the intervention per se (Oei et al., 1996).
- One RCT was excluded from our review because it did not report the full quantitative results of the outcomes (only F-values were provided). Research studies with negative outcomes occasionally fail to provide full results (Heneghan et al., 2017). Also, the RCT that was excluded from our review had some non-significant results regarding anxiety and depressive symptoms. Accordingly, a tendency toward reporting bias exists. Since the search was limited to the English and Korean languages, it is possible that we may have missed some studies in other languages that would otherwise have been eligible for the review. In addition, the exclusion of gray literature from our review may have increased the chance of, or led to, publication bias (McAulely et al., 2000).
- We were unable to measure publication bias due to the small number of included RCTs. As a general principle, tests for funnel plot asymmetry and Egger’s regression test are used when ten or more studies are included in a meta-analysis (Dalton et al., 2016). With such a small number of included trials, all methods for the possible detection of publication bias were underpowered.
- We found a small effect on depressive symptoms of community-dwelling older adults with T2D; however, the effect was not significant. This finding is not consistent with those from a previous meta-analysis. Reviewing studies that examined the effects of CBT on depressive symptoms of community-dwelling older adults regardless of the existence of comorbid chronic disease, Gould, Coulson, and Howard (2012) found a significant greater reduction in depressive symptoms in the intervention group compared to the control. The inconsistent findings may be explained by the difference in the severity of depressive symptoms. The studies included in the meta-analysis by Gould, Coulson, and Howard (2012) specifically targeted depressive symptoms, and therefore, all of the participants had some degree of depressive symptoms. In contrast, having some degree of depressive symptoms was one of the inclusion criteria in only one of the studies included in our meta-analysis, which may have contributed to the small effect size. In all four of the studies included in our meta-analysis, depression scores in the intervention group decreased from baseline to follow-up by an average of 1.2 points, while the control group showed an average decrease of 0.2 points. These findings indicate that CBT-based interventions can be effective in reducing depressive symptoms in older adults living in the community, including those with T2D. However, more studies are needed to draw firm conclusions on the effect of psychological interventions on depressive symptoms in community-dwelling older adults with T2D.
- In relation to blood glucose control, we found that the absolute units of HbA1c from baseline to follow-up were reduced by 1.44% in the intervention group, while the control group showed a decrease of 0.05% from the baseline. These findings are partially consistent with two previous meta-analyses that reported the effects of psychological interventions intended to decrease blood glucose levels in adults (18 years and older) with T2D in a hospital or outpatient setting (Ismail et al., 2004; Chapman et al., 2015). Both meta-analyses showed significant improvement in glucose control. Variants of cognitive behavioral techniques were found to be the most effective and most widely-used psychological interventions for the reduction of blood glucose levels, as compared to other types of psychological interventions, such as motivational interviewing, counseling, and supportive therapy (Ismail et al., 2004; Chapman et al., 2015). These findings indicate that psychological interventions, especially CBT-based interventions, are effective in reducing blood glucose levels, regardless of setting and age range, from young adults to older adults.
- In conclusion, the pooled effect size of community-based psychological interventions for older diabetic individuals in reducing depressive symptoms was not statistically significant, and the effect size was small. On the other hand, a moderate effect size with statistically significant results was found for blood glucose control.
- The overall heterogeneity of the trials was low. As our results indicated, research on psychological interventions for community-residing older diabetic individuals is still in its infancy. The results from our review emphasize the need for studies on psychological interventions for older adults with T2D that have a wider geographical scope (more countries outside the West) and a larger scale to provide more robust evidence.
Discussion
Fig. 3Forest plots of the effect of psychological interventions on depressive symptoms and blood glucose control.


Table 1Descriptive summary of included studies
- 1. Baksi AK, Al-Mrayat M, Hogan D, et al. 2008;Peer advisers compared with specialist health professionals in delivering a training programme on self-management to people with diabetes: a randomized controlled trial. Diabet Med. 25(9):1076-1082. doi:10.1111/j.1464-5491.2008.02542.x.ArticlePubMedPMC
- 2. Beverly EA, Fitzgerald S, Sitnikov L, et al. 2013;Do older adults aged 60-75 years benefit from diabetes behavioral interventions? Diabetes Care. 36(6):1501-1506. doi:10.2337/dc12-2110.ArticlePubMedPMC
- 3. Bogner HR, de Vries HF. 2010;Integrating type 2 diabetes mellitus and depression treatment among African Americans: a randomized controlled pilot trial. Diabetes Educ. 36(2):284-292. doi:10.1177/0145721709356115.ArticlePubMed
- 4. Bond GE, Burr RL, Wolf FM, et al. 2010;The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ. 36(3):446-456. doi:10.1177/0145721710366758.ArticlePubMed
- 5. Chapman A, Liu S, Merkouris S, et al. 2015;Psychological interventions for the management of glycemic and psychological outcomes of type 2 diabetes mellitus in China: A systematic review and meta-Analyses of randomized controlled trials. Front Public Health. 3:252doi:10.3389/fpubh.2015.00252.ArticlePubMedPMC
- 6. Cochrane Collaboration [on-line] Available at http://www.cochrane.org/ Accessed July 2, 2018.
- 7. Dalton JE, Bolen SD, Mascha EJ. 2016;Publication bias: the elephant in the review. Anesth & Analg. 123(4):812-813. doi:10.1213/ANE.0000000000001596.Article
- 8. de Vries HF, Boyle KB, Rooney K. 2016;Diabetes and depression care: a randomized controlled pilot trial. Am J Health Behav. 40(4):503-513. doi:10.5993/AJHB.40.4.12.ArticlePubMed
- 9. Gagliardino JJ, Arrechea V, Assad D. 2013;Type 2 diabetes patients educated by other patients perform at least as well as patients trained by professionals. Diabetes Metab Res Rev. 29(2):152-160. doi:10.1002/dmrr.2368.ArticlePubMed
- 10. Glasgow R, Nutting P, King D, et al. 2004;A practical randomized trial to improve diabetes care. J Intern Med. 19(12):1167-1174. doi:10.1111/j.1525-1497.2004.30425.x.Article
- 11. Gould RL, Coulson MC, Howard RJ. 2012;Cognitive behavioral therapy for depression in older people: a meta-analysis and meta-regression of randomized controlled trials. J Am Geriatr Soc. 60(10):1817-1830. doi:10.1111/j.1532-5415.2012.04166.x.ArticlePubMed
- 12. Heneghan C, Goldacre B, Mahtani KR. 2017;Why clinical trial outcomes fail to translate into benefits for patients. Trials. 18(1):122doi:10.1186/s13063-017-1870-2.ArticlePubMedPMC
- 13. Higgins JP. 2003;Measuring inconsistency in meta-analyses. BMJ. 327(7414):557-560. doi:10.1136/bmj.327.7414.557.ArticlePubMedPMC
- 14. Higgins JP, Whitehead A, Turner RM. 2001;Meta-analysis of continuous outcome data from individual patients. Stat Med. 20(15):2219-2241. doi:10.1002/sim.918.ArticlePubMed
- 15. Hu F. 2011;Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 20:1249-1257. doi:10.2337/dc11-0442.
- 16. Ismail K, Winkley K, Rabe-Hesketh S. 2004;Systematic Review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in pateints with type 2 diabetes. The Lancet. 363(9421):1589-1597. doi:https://doi.org/10.1016/S0140-6736(04)16202-8.Article
- 17. Kirkman MS, Briscoe VJ, Clark N, et al. 2012;Diabetes in older adults. Diabetes Care. 35(12):2650-2664. doi:10.2337/dc12-1801.ArticlePubMedPMC
- 18. Lamers F, Jonkers CC, Bosma H, et al. 2011;Treating depression in diabetes patients: does a nurse-administered minimal psychological intervention affect diabetes-specific quality of life and glycaemic control? A randomized controlled trial. J Adv Nurs. 67(4):788-799. doi:10.1111/j.1365-2648.2010.05540.x.ArticlePubMed
- 19. Markle-Reid M, Ploeg J, Fraser KD. 2018;Community Program Improves Quality of Life and Self-Management in Older Adults with Diabetes Mellitus and Comorbidity. J Am Geriatr Soc. 66(2):263-273. doi:10.1111/jgs.15173.ArticlePubMed
- 20. McAuley L, Pham B, Tugwell P. 2000;Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? The Lancet. 356(9237):1228-1231. doi:10.1016/s0140-6736(00)02786-0.Article
- 21. Mchugh ML. 2012;Interrater reliability: The kappa statistic. Biochem Med. 22(3):276-282. doi:10.11613/bm.2012.031.Article
- 22. Mushtaque A, Gulati R, Hossain MM, et al. 2016;Prevalence of depression in patients of type 2 diabetes mellitus: A cross sectional study in a tertiary care centre. Diabetics Metab Syndr. 10(4):238-241. doi:10.1016/j.dsx.2016.06.016.Article
- 23. Nowlan JS, Wuthrich VM, Rapee RM, et al. 2015;A Comparison of single-session positive reappraisal, cognitive restructuring and supportive counselling for older adults with type 2 Diabetes. Cognit Ther Res. 40(2):216-229. doi:10.1007/s10608-015-9737-x.Article
- 24. Oei TP, Shuttlewood GJ. 1996;Specific and nonspecific factors in psychotherapy: A case of cognitive therapy for depression. Clin Psychol Rev. 16(2):83-103. doi: 10.1016/0272-7358(96)00009-8.Article
- 25. Safren SA, Gonzalez JS, Wexler DJ, et al. 2013;A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in patients with uncontrolled type 2 diabetes. Diabetes Care. 37(3):625-633. doi:10.2337/dc13-0816/-/DC1.ArticlePubMed
- 26. Shirinzadeh M, Afshin-Pour B, Angeles R, et al. 2019;The effect of community-based programs on diabetes prevention in low- and middle-income countries: a systematic review and meta-analysis. Global Health. 15(1):10doi:10.1186/s12992-019-0451-4.ArticlePubMedPMC
- 27. Sjostrom L, Peltonen M, Jacobson P, et al. 2014;Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 311(22):2297-2304. doi:10.1001/jama.2014.5988.ArticlePubMed
- 28. Taveira TH, Dooley AG, Cohen LB. 2011;Pharmacist-led group medical appointments for the management of type 2 diabetes with comorbid depression in older adults. Annals of Pharmacotherapy. 45(11):1346-1355. doi:10.1345/aph.1q212.ArticlePubMed
- 29. Weiss DM, Casten RJ, Leiby BE. 2015;Effect of behavioral intervention on dilated fundus examination rates in older African American individuals with diabetes mellitus. JAMA Ophthalmology. 133(9):doi:10.1001/jamaophthalmol.2015.1760.Article
- 30. World Health Organization. 2016 A report on Diabetes Retrieved from https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf?.sequence=1
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Factors Affecting Bereaved Spouses’ Quality of Life: A Systematic Review
Wonjung Noh, Songi Jeon
Stress.2020; 28(4): 254. CrossRef




 PubReader
PubReader Cite
Cite